What Can an EM Union Do For You?
Unionization is no silver bullet, but does give emergency clinicians more negotiating power in intriguing ways.
Emergency medicine had a rough 2023.
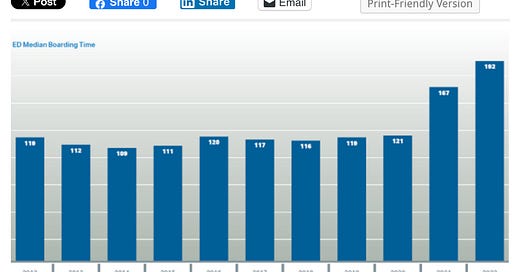
Two of the five largest emergency medicine practices in the US declared bankruptcy. The biggest hospital system in the US got sued by the state of North Carolina for mismanaging its emergency department. Boarding times accelerated due to hospital understaffing. Insurance companies are using the No Surprises Act to underpay EM practices. Emergency physicians' real wages (adjusted for inflation) decreased for the fifth consecutive year. EM had the highest burnout rate and the lowest job satisfaction in the House of Medicine. Female emergency physicians left the specialty at alarming rates. Medical students noticed, leading to decreases in the number applying to emergency medicine residencies.
Looking forward to a new year, how can we reinvigorate this once-proud specialty? Some emergency medicine leaders are exploring whether unionization can provide the structure and legal protections for such a turnaround. Let’s dive into how a union of employed emergency physicians, PAs, and nurse practitioners could improve working conditions in EM. (For a more general discussion of physician unionization, check out last week’s EM Workforce Newsletter.)
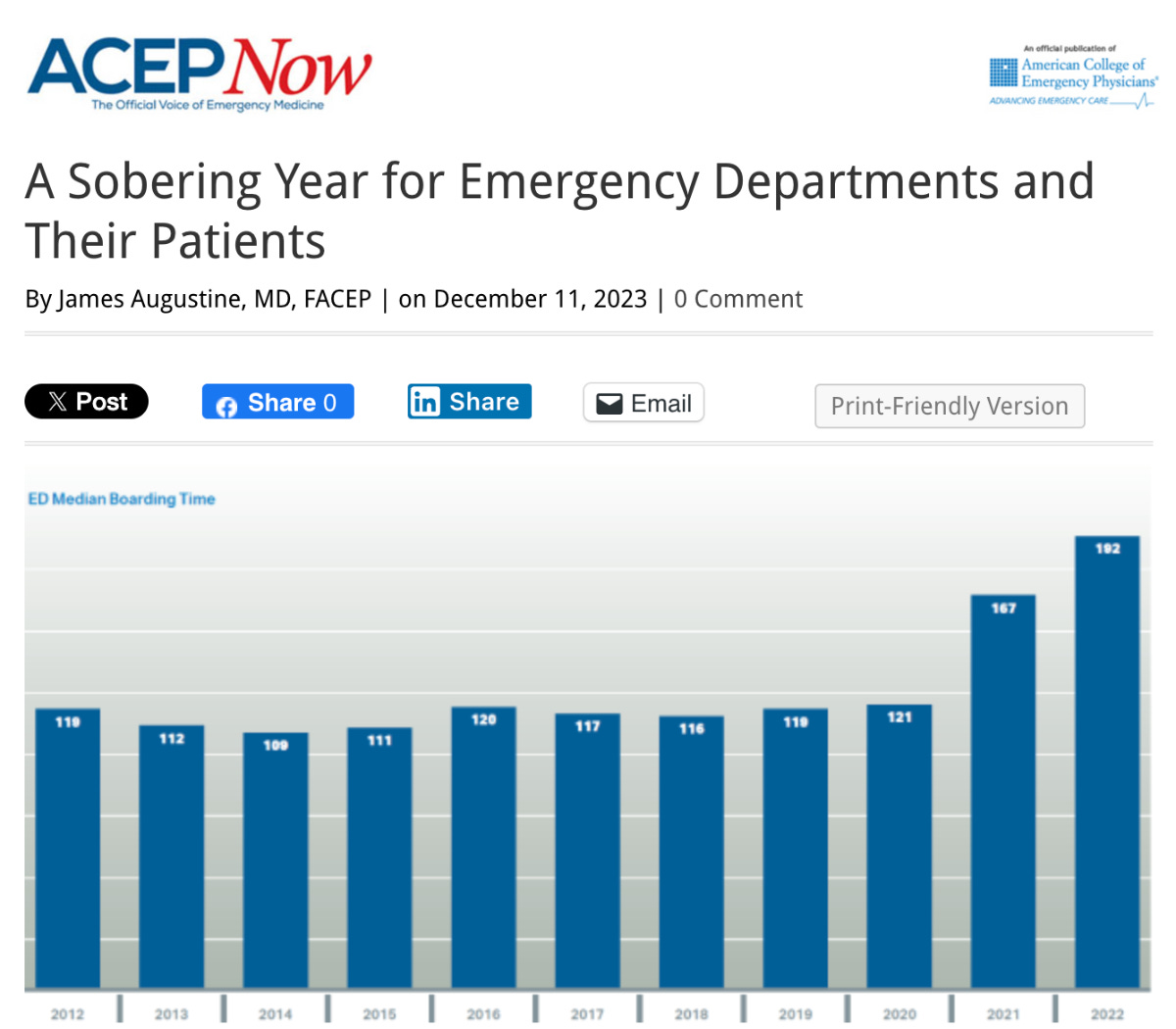
Most emergency physicians are employed within a three-tiered structure. The base layer is the corporation that legally staffs the emergency department and bills insurance companies. You can look up this entity's name for any ED through Medicare’s Care Compare website. Envision Healthcare’s many subsidiary entities are listed in the diagram below from the company’s 2023 bankruptcy filings.
The next layer is the parent company, such as TeamHealth, SCP, or US Acute Care Solutions. The emergency department I work at - Wilson Medical Center - is staffed by Emergency Coverage Corp, a TeamHealth subsidiary.
The hospital or health system is the third layer. Though most hospitals outsource their emergency physician workforce, they meet the National Labor Relations Board criteria for “joint employers.” Per the National Federation of Independent Businesses, “a business, other than the main employer, will be considered a joint employer if it has any authority to control the following employment terms: Wages, benefits, and other compensation; Hours of work and scheduling; The assignment of duties to be performed; The supervision of the performance of duties; Work rules and directions governing the manner, means, and methods of the performance of duties and the grounds for discipline; The tenure of employment, including hiring and discharge; and Working conditions related to the safety and health of employees.”
This three-tiered employment structure would allow an emergency physician union to bargain with each of the three employer entities. The union could negotiate for proper compensation from clinicians’ direct employers and, more importantly, for improved working conditions at their hospital.
Boarding is the most pressing working condition problem in most US hospitals. ED boarding results from hospitals’ understaffing of inpatient medical and psychiatric units. An emergency physician union can join nursing unions such as National Nurses United in their advocacy for legally mandated staffing levels. Without a union, physicians and emergency medicine groups risk their jobs and contracts when advocating for issues potentially harmful to their hospitals’ profits.
If state legislative advocacy is ineffective, the union could take more direct action to motivate hospitals to staff their medical and psychiatric units appropriately. One could imagine a campaign similar to the pre-pandemic hospital roadside billboards showing ER wait times. Instead of listing door-to-clinician time, the EM union billboards would display the ED’s longest current boarding time (measured in days? weeks?) - including psychiatric holds. Creative campaigns about workplace safety and quality of care concerns could also be imagined.
Union members are protected from being fired as a result of advocating for improved working conditions. And if the hospital changes emergency medicine contractors, the union would likely remain (unless the practicing physicians own the incoming group). The due process protections that Dr. Robert McNamara, AAEM, and others have been championing for decades would finally be in place.
Collective bargaining with the primary emergency medicine employer would be more straightforward. Issues such as protections in case of employer bankruptcy, revenue sharing, compensation structures, and staffing skills mix would be expected elements of the negotiations.
The American Physician Partners bankruptcy showed emergency clinicians the precarious state of their employment. APP shut down operations with less than one month’s notice, leaving physicians unpaid for that month’s work and with their malpractice tail uncovered. Collective bargaining can help ensure that workers are better protected in future bankruptcies.
Preparations for possible bankruptcies are not a minor consideration. TeamHealth’s debt is rated CCC- by Fitch, meaning “a very high level of default risk.” In August, S&P Global Ratings downgraded Sound Physicians’ credit rating from B- to CCC, citing the company’s “weak financial performance and cash flow, very high leverage and low trading levels.”
Emergency physicians are generally not allowed to see their employers’ financial details, such as revenues and expenses. However, during collective bargaining, a union is entitled to an employer’s financial information when an employer bases its bargaining position on an asserted inability to pay. This is based on a 1956 Supreme Court case that concluded, “In the circumstances of this case, where the employer claimed that it could not afford to pay higher wages but refused the union's request to produce financial data to substantiate this claim, the National Labor Relations Board was justified in finding that the employer had not bargained in good faith and, therefore, had violated 8 (a) (5) of the National Labor Relations Act. Pp. 149-154.”
In a business that generates revenue exclusively through physician, PA, and nurse practitioner clinical work, a union would have a strong case for clinicians to retain a large share of that revenue.
How clinician compensation is structured would be an expected part of collective bargaining. Due to emergency physicians’ three-tiered employment, compensation structures can be negotiated anywhere from the site level to the whole employer level, depending on the parties' preferences. Topics for negotiation would include paid parental leave, compensation for meeting attendance & committee involvement, night differentials, rural-urban site pay differentials, scribe program funding, and performance incentives.
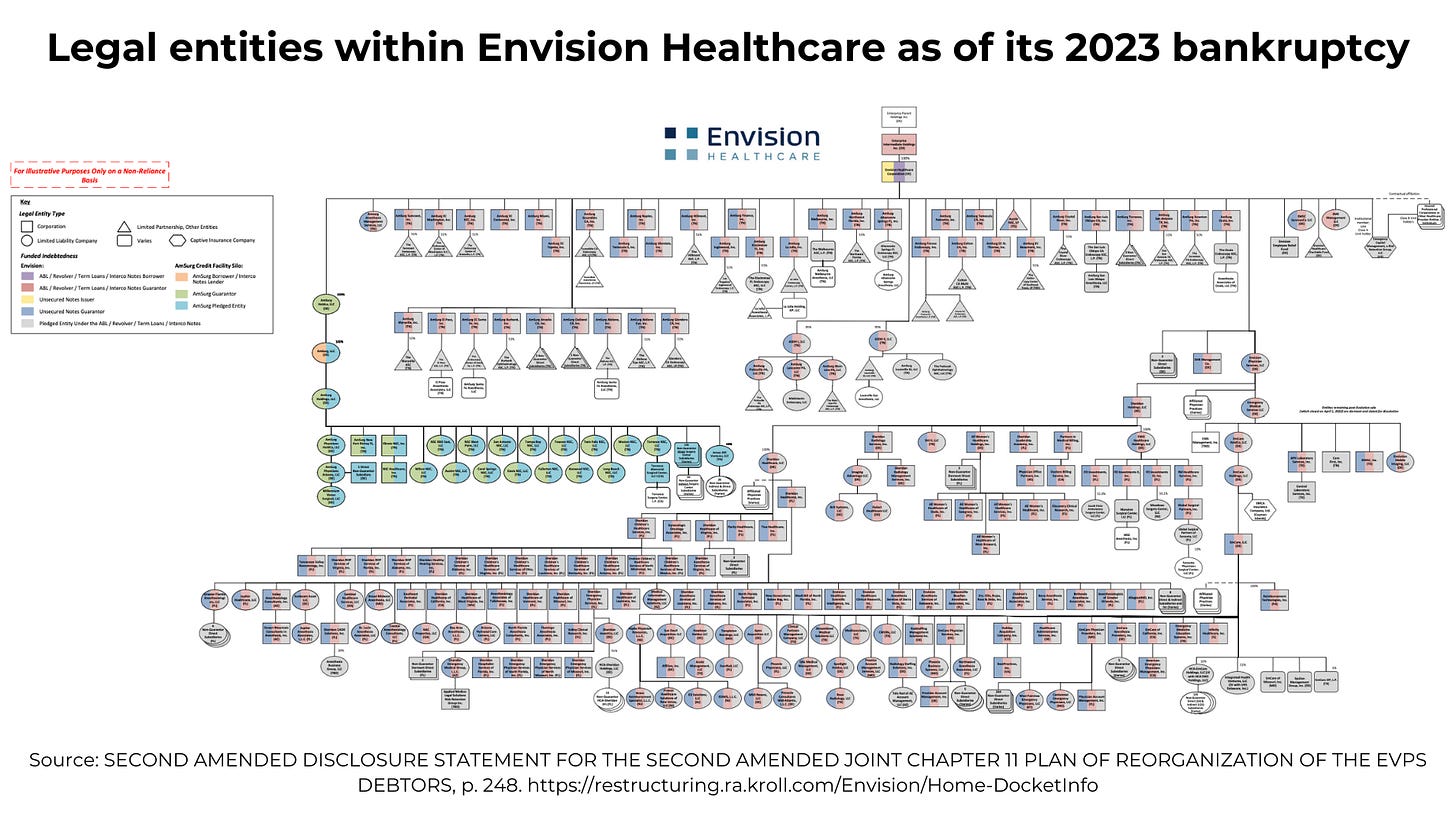
An additional compelling topic for negotiations would be the skill mix within the emergency medicine group. Employers are financially incentivized to maximize the number of PAs and nurse practitioners compared with physicians - even in states that do not allow independent NP practice. A clinician union would be expected to negotiate for a ratio of physicians to PAs & nurse practitioners optimal for delivering high-quality, efficient patient care.
Engaging in collective bargaining with an emergency clinician union would not be seen favorably by the employer group or by the hospital. Current information and power asymmetries between large groups and individual clinicians strongly favor employers. Health system administrators do not want legally protected physicians criticizing their hospital in public or negotiating for changes that are not in the hospital’s financial interests.
The likely outcome of emergency medicine clinicians who work for outsourced employers forming a union would be for hospital administrators to find legal ways to dissolve the union. The most effective strategy for doing so would be to contract with an EM group owned by its practicing clinicians. Owners cannot unionize so the union would be eliminated.
Unionization is an intriguing path to success for those looking to return control of emergency medicine practices to working physicians. Let’s see if 2024 becomes the “Year of the EM Union,” kick-starting the rejuvenation of emergency medicine.






"There are no silver bullets for this, only lead bullets.”
https://a16z.com/lead-bullets/