Decreasing Real Wages for Emergency Physicians
Also: Return of the 3-Day Rule, SAVE Act reintroduced, hospital bigs get bigger, & nurses join the gig economy.
Top of the Week
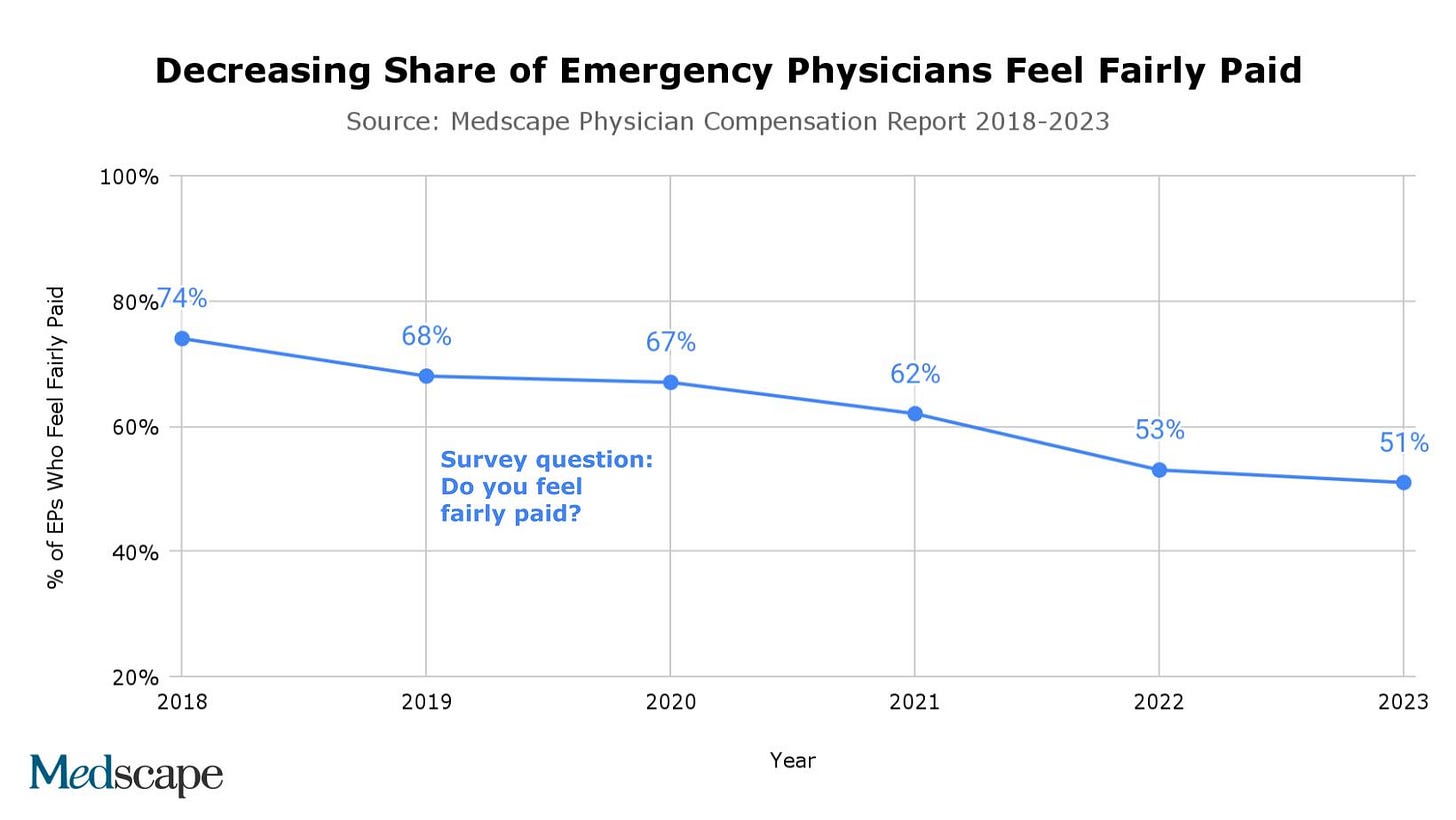
Practicing emergency medicine is challenging. Surveys from a few years ago showed that most emergency physicians felt the degree of difficulty was balanced by relatively high wages. In 2018, 74% of emergency physicians felt fairly paid. No longer. In the 2023 Medscape Physician Compensation Report, only 51% of EPs feel they are compensated fairly - a decrease of 23% in five years.
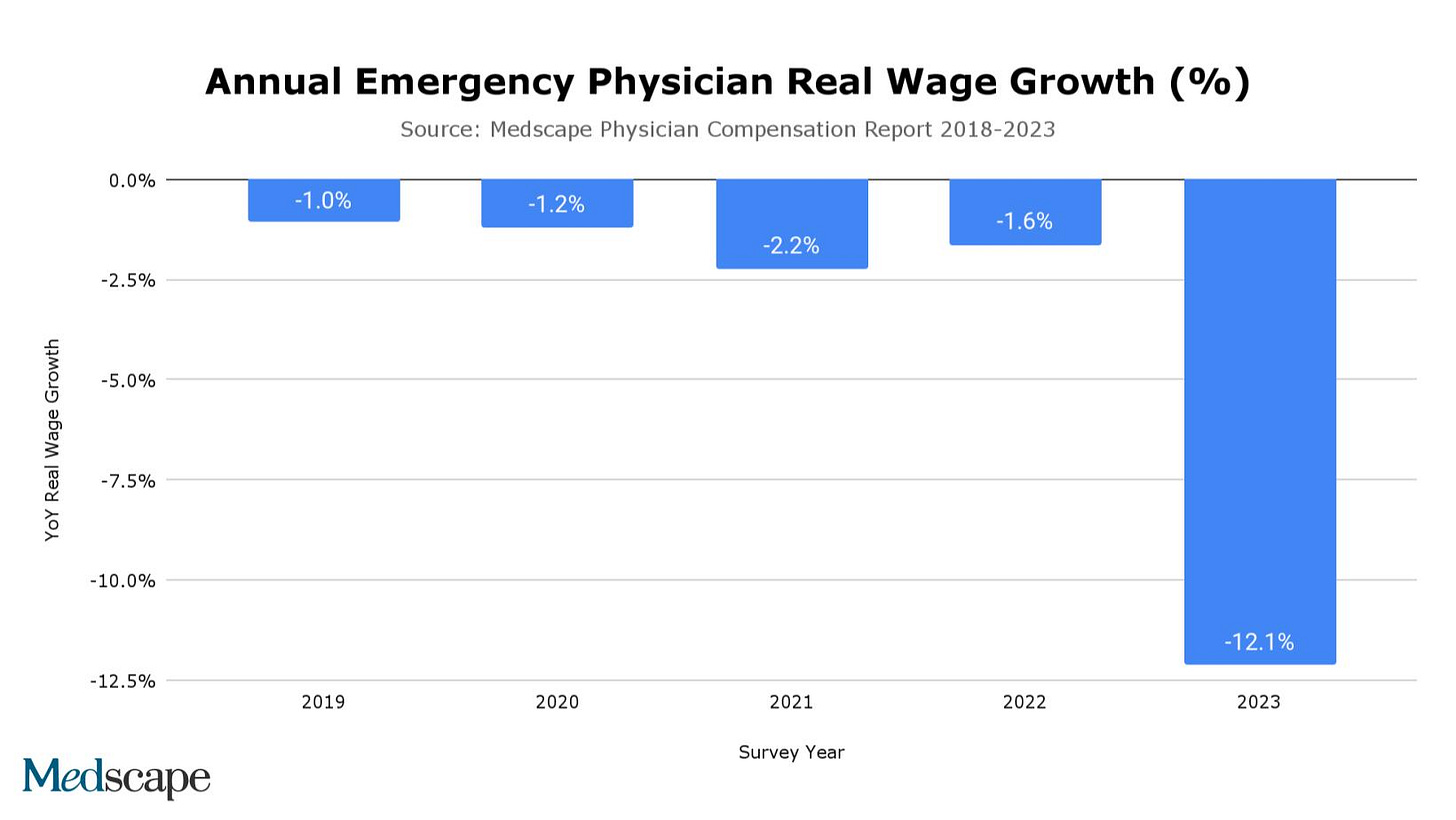
The perception of lower EP compensation is backed by the data. In each Medscape survey from the last five years, annual changes in emergency physician real wages (compensation increase adjusted for inflation) have been negative.
The year going into the 2023 survey - conducted at the end of 2022 - had the most strikingly negative real wages change for emergency physicians, at -12.1%. How can this be explained?
No Surprises Act. The NSA went into effect in on January 1, 2022. The law barred medical practices from billing out-of-network, decreasing reimbursement from bills that transitioned from higher out-of-network rates to lower in-network rates. Insurers have also used the NSA as reason to remove high-paying contracts from their networks, aiming to decrease future market rate averages. Meanwhile, the NSA’s arbitration system has had many delays and costs, further depressing collections from private payers.
Distributions within practices. Emergency medicine has seen rapid consolidation over the past decade. In the typical buyout, whether financed by private equity, the health system, or through debt, the selling physicians receive significant payouts that span several years. However, once the purchase is complete, the buyer is incentivized to decrease compensation. To achieve profitability, the group needs to to recoup their purchasing costs and pay down the financing used for the acquisition. Physician wages are the biggest expense of consolidated medical practices.
Lack of increase in government payer rates. The 2022 Medicare conversion factor was slightly lower than in 2021, while the RVU values were held relatively flat.
Inflation. Purchasing power in the United States has decreased more in the past two years than at any time since the 1980s. The year-end consumer price index increase was 6.5% in 2022 and 7.0% in 2021.
EM Practice
The 3-day rule for Medicare coverage of discharges to skilled nursing facilities will be reinstated on May 11, when the public health emergency ends.
University of Alabama at Birmingham: “Emergency department crowding has reached a crisis point.”
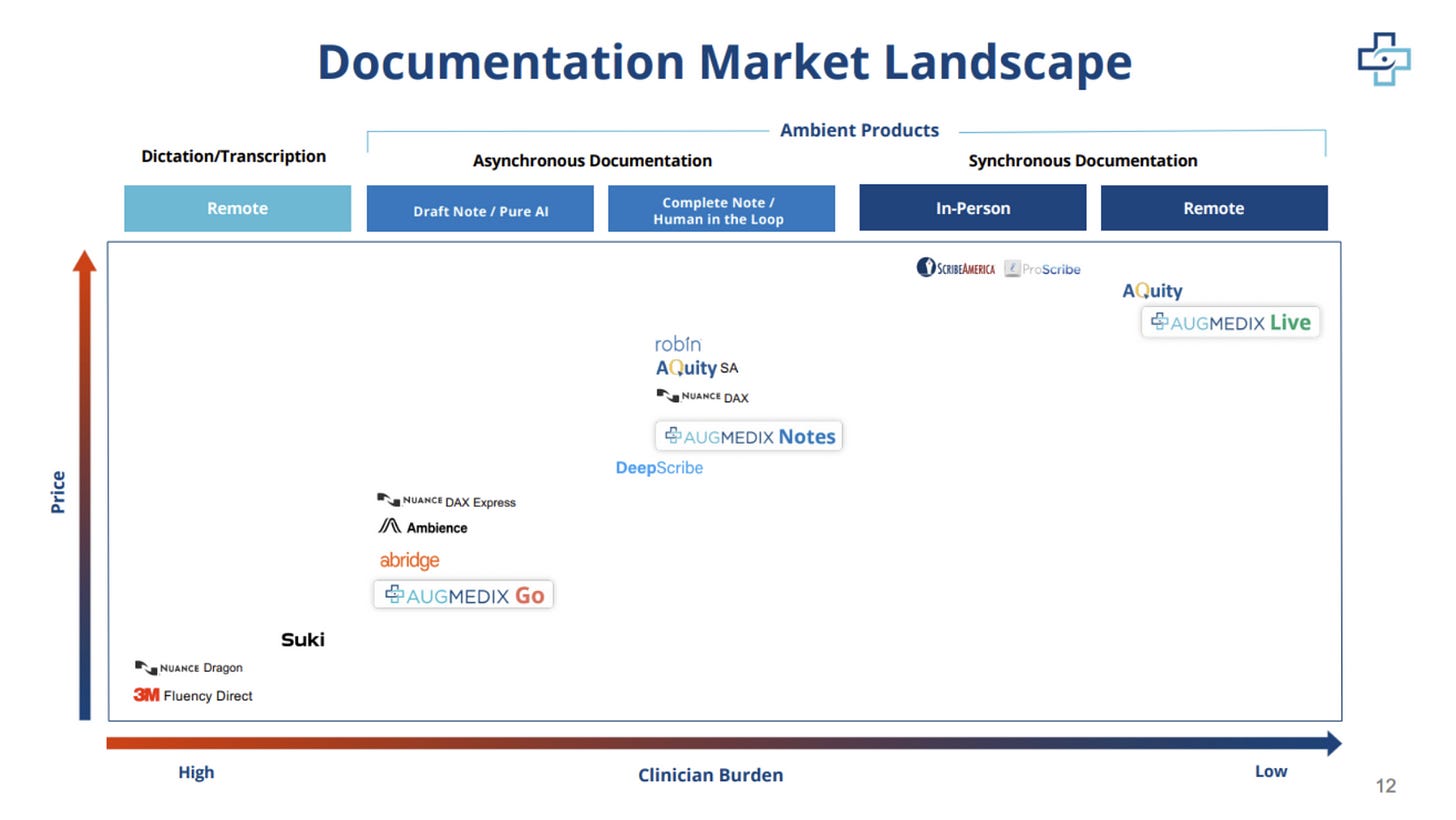
EM documentation technology is advancing rapidly. Check out this Blake Madden interview with Augmedix founder Ian Shakil.
House of Medicine
Several states’ attorneys general are urging the FTC to ban non-competes. “A federal rule limiting non-competes will significantly benefit workers and promote fair competition among businesses.”
The Safety from Violence for Healthcare Employees (SAVE) Act was reintroduced in the US House of Representatives. “This bill, which is modeled after current protections for aircraft and airport workers like flight crews and attendants, would create legal penalties for individuals who knowingly and intentionally assault or intimidate hospital employees.”
Hospitals & Health Systems
Kaiser Permanente announced plans to buy Geisinger Health. The new entity will be called Risant Health. Kaiser aims to purchase several other “like-minded, nonprofit, value-oriented community-based health systems” under the new Risant Health structure.
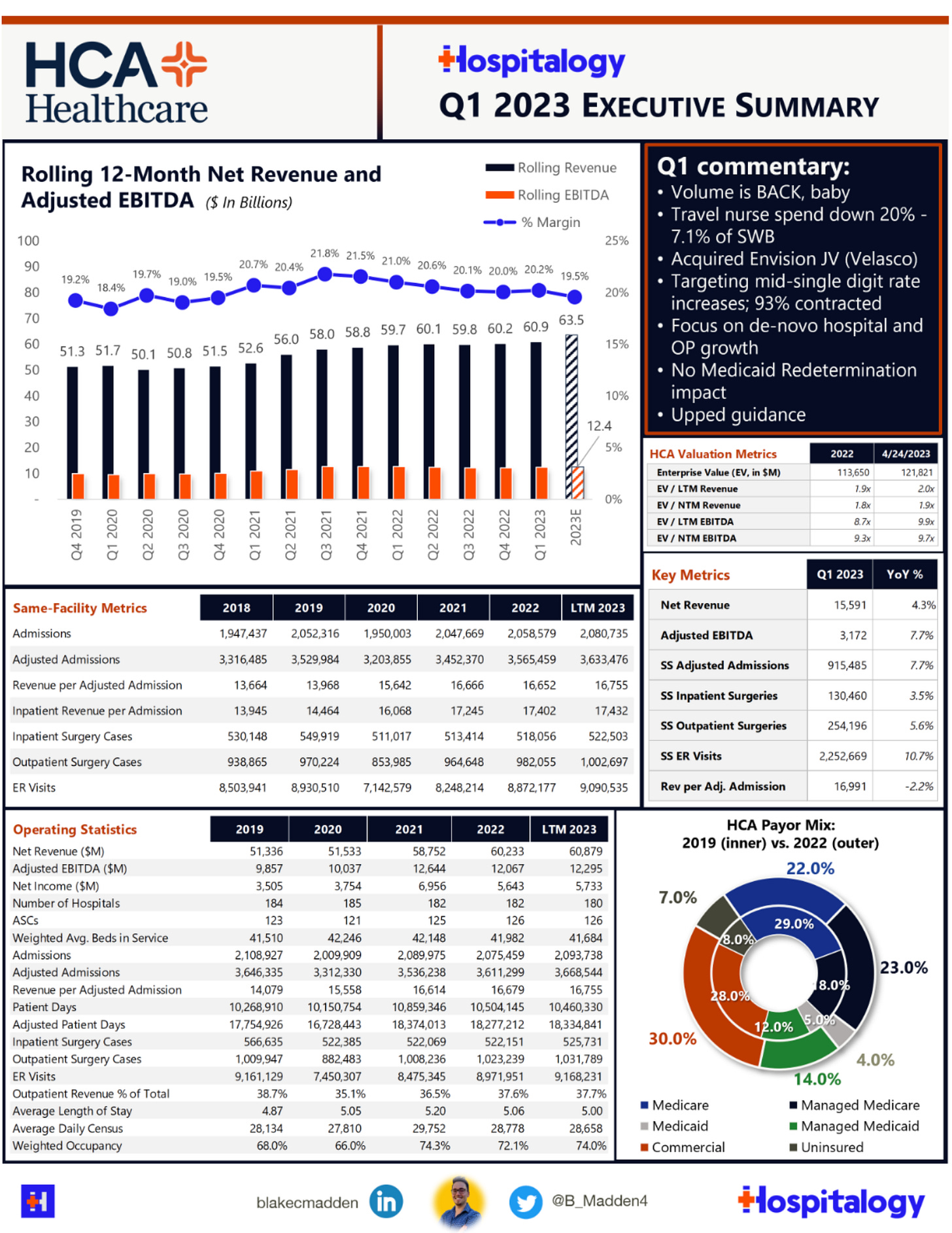
HCA Healthcare not only increased earnings in Q1 2023; it also saw a 10.7% year-over-year increase in ED volume.
Tenet’s and UHS’ balance sheets are also improving.
Post-mortem after the closure of Atlanta Medical Center, a 460-bed urban hospital.
Nursing & Allied Health
In-depth interviews of hospital staff about working through the COVID years.
Washington State has passed a law increasing nurse staffing standards for hospitals.
How technology has impacted nursing, bringing the field into the “gig economy” (WSJ article).
The Dispo
Tweet of the week.




Always pains me when doctors complain about not making enough money, when even the lowest-paid physicians (pediatricians, internists, FPs) make three to four times the annual income of the average (median) American family. But any time comp goes down, people feel the pain, and with costs of everything going up, the squeeze hits us too. The abusive practice of billing emergency patients at out-of-network rates and despite (or because of) their non-covered status needed to come to an end. Any physician who was a party to that abuse should be ashamed (if such a vestige of human decency remains). The article also does a good job of outlining other factors in the salary squeeze; it does not look like these will be reversing any time soon.