What happens when we can see each other’s salaries?
Also: Emergency physician burnout rate increased to 65% in 2022, healthcare defaults are predicted for 2023, and attendings aren’t great at predicting blood alcohol levels.
Top of the Week
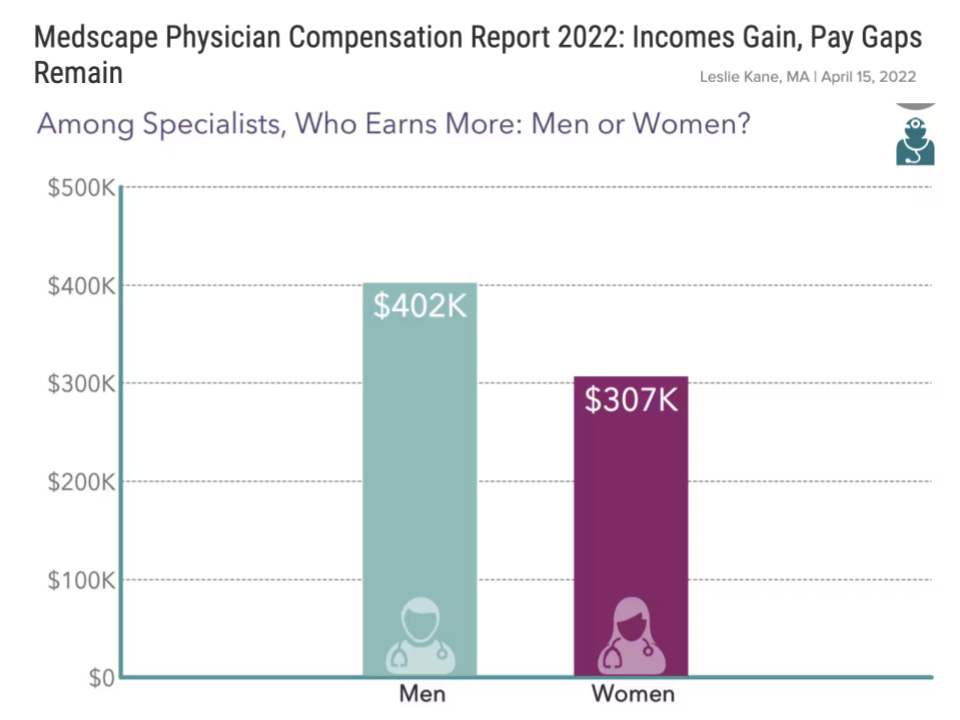
Women and minorities have long been underpaid in healthcare, as in other industries. A Health Affairs article from December 2021 showed that, based on a large salary data set, a female physician over a 40-year career earns approximately $2 million less than a comparable male physician.
“Pay transparency laws are very good at reducing wage disparities”, per Zoe Cullen, an economist at Harvard Business School. As a result, pay transparency has become an increasingly common tactic to address pay disparities. This month, California and Washington joined Colorado and New York in requiring companies to include salary ranges in their job postings.
Studies of pay transparency have found an interesting pattern: decreased pay variation, but also modestly lower total compensation and increased productivity. If this pattern holds, employers may actually benefit from salary transparency.
A 2022 Nature Human Behavior study of 100,000 US academics concluded that “pay transparency causes significant increases in both the equity and equality of pay, and significant and sizeable reductions in the link between pay and individually measured performance.” Per another study, “When pay systems are perceived as fair, pay transparency is associated with lower turnover rates. When it is perceived as unfair, the opposite is true.”
Data showing a slight decrease in overall compensation as a result of salary transparency comes from an NBER paper. The authors explain, “Our model predicts that transparency reduces the individual bargaining power of workers, leading to lower average wages.”
EM Practice
Emergency physician burnout increased in 2022 compared with 2021. 65% of EPs were burned out, per Medscape, topping all specialties. The Advisory Board discusses ways to address physician burnout.
ACEP is seeking comments and ideas about parental leave for emergency physicians.
MetroWest Medical Center in Framingham, MA has brought in TeamHealth to replace its single-site emergency medicine group.
Financial Times article discussing the challenges of debt-laden healthcare staffing companies such as Envision. “‘What we’re hearing about now in the US healthcare space is labour pressure, wage pressure from employees demanding higher wages, at the same time that government reimbursement rates for some of the names in the healthcare space are lagging,’ said Caprio. Together with the weight of rising interest rates, such pressures could make it more difficult for companies to access fresh funding just as a darkening economic backdrop threatens to hamper revenue growth — paving the way for a flurry of downgrades and defaults in 2023. ‘Finding lenders willing to refinance will become increasingly difficult in the year ahead as the market retrenches,’ Moody’s said.”
House of Medicine
The Texas Medical Association filed its fourth lawsuit over the No Surprises Act. This suit challenges the 600% hike in administrative fees for seeking federal dispute resolution.
A new industry is growing to support the administrative aspects of independent medical practices.
Hospitals & Health Systems
A JAMA analysis of health system performance compared with independent providers concluded: “Performance on clinical quality and patient experience measures was marginally better in systems but spending and prices were substantially higher. Small quality differentials combined with large price differentials suggest that health systems have not, on average, realized their potential for better care at equal or lower cost.”
Deep dive into the hospital-at-home model of care.
HCA Healthcare posted a $5.6b profit in 2022.
Emerus, which operates micro-hospitals, has surpassed three million patients treated.
Another rural hospital has closed.
Nursing & Allied Health
The US Department of Justice uncovered a Florida-based scheme to sell fraudulent nursing diplomas.
Staffing shortages are causing lots of problems at Ascension Columbia St. Mary's Hospital in Milwaukee.
The Dispo
A new study shows that nurses and residents were better than attending emergency physicians at predicting inebriated patients’ blood alcohol levels. Clinicians tended to overestimate patients’ BALs.