NFL Players' Unionization Playbook for Emergency Physicians
Also: Sage advice for young EPs, NYP Columbia ED gets the "Name and Shame" treatment, the Ballad of healthcare monopolies, Kaiser on strike, & Taylor Swift.
Thomas Cook, MD, titled his most recent EM News column, “Why Do EPs Feel Powerless?” The answer: most emergency physicians feel powerless because most EPs are professionally powerless.
Emergency physicians could use a playbook on how to regain power. Some argue that fighting the corporate practice of medicine is the right strategy for empowerment. The American Academy of Emergency Medicine (AAEM) has been battling non-physician ownership of EM practices since 1993. In that time, physician practice ownership rates have plummeted. When a strategy doesn’t work for thirty years, it is probably time to look for new ideas.
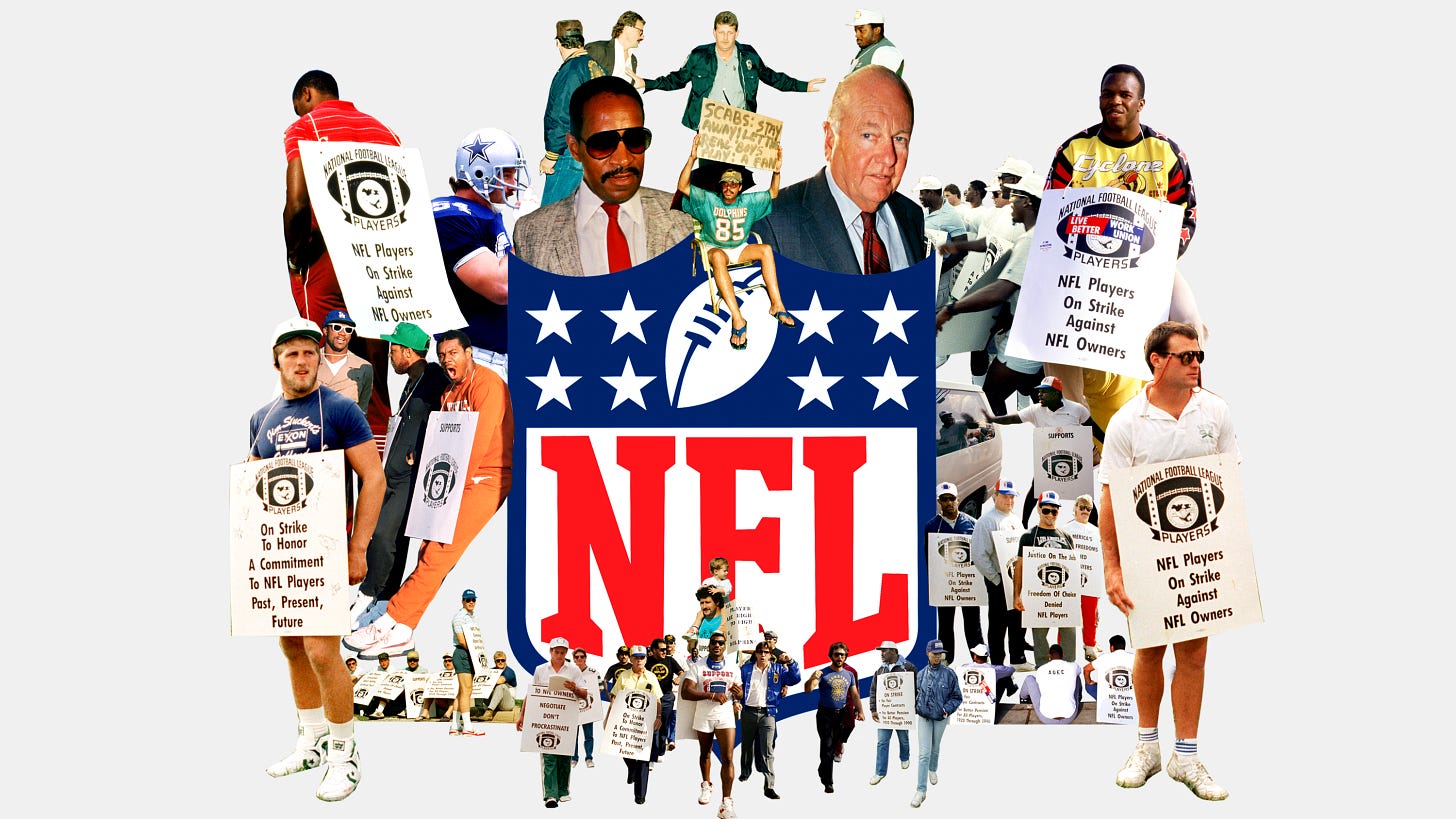
Hard as it is to believe, until the late twentieth century, pro football players were also relatively powerless. In the early years of the NFL, football players were not even guaranteed clean uniforms. Pro athletes were forced to play the preseason and exhibition games for free, risking career-ending injuries.
Tired of being taken advantage of, a group of players, including Don Shula and Frank Gifford, formed the NFL Players Association (NFLPA) in 1956. Every team except the Chicago Bears joined. Negotiating together, the players not only won clean uniforms but also received a salary minimum of $5,000 per season, $50 per exhibition game, and health insurance.
The NFLPA explains, “Legend has it that the NFL Players Association was born out of a simple demand: clean socks and jocks. Truth be told, pro football players wanted a little more than that when they formed the union in 1956; they wanted a voice.” As a result of a series of negotiations punctuated by strikes, lock-outs, and lawsuits, the players gradually gained more power.
By the 70s, free agency became players’ top priority. Owners were not incentivized to pay players fairly without the risk of players leaving to work for another team. Because this arrangement was so profitable for owners, negotiations over free agency were unsuccessful.
The NFLPA then turned to the courts. In a landmark case, Reggie White, representing all NFL players, led a class action lawsuit against the league to obtain free agency rights. On September 10, 1992, the federal court sided with the players, ruling that NFL restrictions on players changing teams violated antitrust laws. The impact was immediate; average NFL wages increased by 38% the following season.
How successful has the NFLPA been at empowering and protecting its union members? One answer is financial. As a result of the 2020 collective bargaining agreement, players are guaranteed at least 48% of league revenues. Teams are mandated to send a copy of every player's contract to the NFLPA to ensure compliance. In 2022, the NFL generated approximately $18.6 billion.
The Damar Hamlin case illustrates another answer. At 8:55 pm on Monday, January 2, 2023, Damar Hamlin, a Buffalo Bills safety, made what initially appeared to be a routine tackle of a Cincinnati Bengals player. As Hamlin stood up, he wobbled and then collapsed. Hamlin was pulseless.
The NFL’s emergency action plan was activated immediately. Within 10 seconds, CPR was initiated by Bills' team physicians and trainers. Hamlin was defibrillated on the field. Within five minutes, he was placed in an on-field ambulance and intubated. Hamlin was transported to the University of Cincinnati Medical Center. After nine days in the hospital, Hamlin was discharged in good condition. He is back playing professional football with the Buffalo Bills.
The impressive resuscitation was no accident. The football game’s emergency action plan had been negotiated in detail by the NFLPA. The 2020 NFL Collective Bargaining Agreement (CBA) is 456 pages long, including 70 pages about “players’ rights to medical care and treatment.”
The NFLPA’s Medical Director - currently emergency physician Thom Mayer, MD - is a voting member of all NFL health and safety committees. Additionally, the NFL has a Chief Medical Officer. Every team must have a designated orthopedic surgeon, a primary care sports medicine physician, and a neurologist. An emergency action plan is mandated for every team.
Per the CBA, “The parties shall jointly select an expert in the field of emergency medicine (the “EAP Expert”) to help them establish minimum standards, protocols, and a standardized format for an Emergency Action Plan (“EAP”) that shall be required to be submitted by every NFL Club to address player medical, cardiac and/or surgical emergencies that occur at games hosted at their home stadium, as well as at the practice facility (if different from the game day venue)... The parties (through the NFL Chief Medical Officer and the NFL Players Association Medical Director) must review all EAPs prior to the start of the season. The EAP requirements shall be published to every NFL Club prior to March 15 of each year to ensure that Club medical staffs have adequate notice of any changes.”
When most Americans think of unions, the UAW or the Teamsters come to mind. However, the NFLPA is more applicable to emergency medicine. Pro football players have a unique skill set that is highly valued by society. The industry is closely regulated. It cannot be exported or replaced by machines.
A key difference is that while football players were always “labor” working for a separate group of owner employers, physicians traditionally were both the workers and the owners. Now that most emergency physicians are “labor,” turning back the clock and regaining physician practice ownership at scale is unlikely. The NFL Players Association shows that through solidarity, collective bargaining, and professional excellence, a group of employed workers can gain impressive amounts of power while enabling their industry to thrive.
EM Practice
From EMResident: “Advice to Senior EM Residents (actually, all residents & fellows)” by Dr. Gus M. Garmel, MD, FACEP, FAAEM. “Given how changes in the EM landscape are continuous and rapid, my first suggestion is to be present and pay attention. Be present in your interactions with your patients and colleagues. Pay attention to the political climate in EM (at national and state levels), to organizations in EM, and to the business of EM (nationally and locally). Give intentional attention to these areas, in addition to scientific advances in our field. This knowledge will prove relevant throughout your career, which, despite its challenges, will hopefully be productive, lengthy, and satisfying.”
Post about the rough working conditions at the NewYork-Presbyterian Columbia University Irving Medical Center emergency department.
Summary of the House of Representatives hearing about the No Surprises Act. “The law called for a dispute resolution process for medical providers and insurers, overseen by independent mediators, to negotiate a fair payment for surprise or out-of-network services given to patients. So far, that fair system has not been implemented, and multiple lawsuits have plagued the process with unpredictable starts and stops while medical providers are waiting to receive payments from insurance companies, even after a dispute has been resolved.”
House of Medicine
US Bureau of Labor Statistics: How much do PAs make in each state?
AMN survey of final year residents.
From PhysicianOnFire.com:
Nursing & Allied Health
75,000 Kaiser Permanente workers went on strike this morning, making it the largest healthcare strike in US history.
Hospitals & Health Systems
Local governments are noticing that nonprofit hospitals are acting more like for-profit hospitals. As a result, some are looking to claw back non-profit hospitals’ tax breaks.
Why are Amazon, Walgreens, and CVS spending billions on primary care clinics? To capture prescription sales through their pharmacies.
Monopolies are good for monopolists, but usually harmful to the public. KFF explores the results of Ballad receiving regional monopoly rights.
CEO of the Cedars-Sinai Health System in Los Angeles on cost-shifting, published in Health Affairs. “Going forward, commercial insurance payments will have a profound impact on the nature, size, and adequacy of the hospital and physician delivery system. Inadequate Medicare and Medicaid funding and other relevant market factors must be considered in commercial pricing decisions.”
KaufmanHall report: US hospital operating margins are improving.
The Dispo
Can’t write about the NFL without a Taylor Swift cameo…
Emergency Medicine Workforce Productions is sponsored by Ivy Clinicians - simplifying the emergency medicine job search through transparency.