New Hampshire Had Zero Involuntary ED Mental Health Boarders - for a Day
A federal judge ruled in 2023 that ED boarding of psychiatric admissions in NH is unconstitutional under the US Constitution's 4th Amendment, leading to the state's "Mission Zero" initiative.
The New Hampshire Department of Health and Human Services (DHHS) announced that on December 6, 2024, no adults admitted for involuntary inpatient mental health treatment were waiting in an emergency department rather than being transported to a psychiatric hospital. This was a dramatic improvement from a year prior, when 32 admitted mental health patients were boarding in New Hampshire EDs.
Combating long waits for mental health care has become a high priority for New Hampshire’s state government. “We are hitting the gas more than we really ever have, on any issue, when it comes to this effort,” said Morissa Henn, the deputy commissioner of New Hampshire’s DHHS.
Why and how did New Hampshire address its behavioral health ED boarding problem? What are the prospects for sustained progress? Let’s dive in.
Psychiatric Boarding Declared Unconstitutional by Federal Court
On February 23, 2023, Judge Landya B. McCafferty ruled that the New Hampshire Department of Health and Human Services violated hospitals’ Fourth Amendment rights through the prolonged boarding of involuntarily committed mental health patients in emergency departments. The hospitals’ winning argument in this case is compelling and original.
The Fourth Amendment to the US Constitution states, “The right of the people to be secure in their persons, houses, papers, and effects, against unreasonable searches and seizures, shall not be violated, and no Warrants shall issue, but upon probable cause, supported by Oath or affirmation, and particularly describing the place to be searched, and the persons or things to be seized.”
The hospitals argued that their emergency departments are required by law to deliver emergency mental health treatment. Patients with acute psychiatric illnesses are evaluated in EDs for their level of danger to themselves or others. Those deemed to be at high risk are certified for involuntary emergency admission ("IEA") to the state's mental health services system.
Although physicians conduct the IEA certification process in private hospitals, they do so as part of the state mental health system. “Once the IEA certificate is complete, by operation of law, the IEA-certified patient becomes the Commissioner's patient in the state's mental health services system.”
New Hampshire regulations stipulate that the “IEA certificate must identify the receiving facility and the patient must be delivered immediately to the facility identified in the certificate." However, the judge noted that “the process breaks down at this point because the immediate transfer is not occurring in most cases.”
The hospitals submitted details to the court about extended waiting times for mental health admissions. Each of the hospitals in New Hampshire had “IEA-certified patients waiting for days in their emergency departments for space to open in a designated receiving facility.” While those patients are kept involuntarily in hospitals’ emergency departments, those health systems are compelled to shelter and care for the patients, thereby incurring significant costs. The hospitals receive no payment from the state for caring for uninsured mental patients admitted to the state hospital.
The judge concluded, “The Hospitals have established that the Commissioner's practice of boarding IEA-certified patients in the Hospitals' emergency departments has violated and continues to violate their Fourth Amendment right to be free from unreasonable seizures of their emergency departments.”
On May 17, 2023, Judge McCafferty ordered that:
The Commissioner of the New Hampshire Department of Health and Human Services is permanently and prospectively enjoined from seizing the hospitals’ property and resources in violation of their Fourth Amendment rights by failing to accept the transfer of IEA patients to a designated receiving facility as soon as is practicable but no later than 6 hours after the transmittal of a completed IEA Certificate by a hospital to the Department.
The Commissioner shall be in compliance with this injunction within 12 months of the date of this order.
The state of New Hampshire was on the clock to end mental health boarding.
Mission Zero
As of June 2023, 31 patients per day, on average over the prior year, had been waiting for involuntary psychiatric admissions in New Hampshire. Reducing that number to near zero would be a monumental task.
After the court ruling, the New Hampshire Department of Health and Human Services launched “Mission Zero” to address the ED boarding crisis. The initiative focused on adding more inpatient psychiatric care capacity, improving community-based mental health services, and creating more housing options for people with serious mental illness.
Mission Zero’s specific interventions included:
Expansion of Certified Community Behavioral Health Clinics,
Investing in Community-Based Crisis Stabilization Centers,
Implementing a Care Traffic Control System,
Expansion in Designated Receiving Facility beds,
Increasing care capacity in step-down and less restrictive settings, and
Creation of landlord incentives to expand places to remain stably housed.
See the image below for a detailed set of plans, including the state funds allocated for each element of the Mission Zero initiative as of February 2024.
Challenges Remain
A single day without involuntary mental health boarding in New Hampshire is an accomplishment. However, Mission Zero’s success may be unsustainable without additional resources and funding.
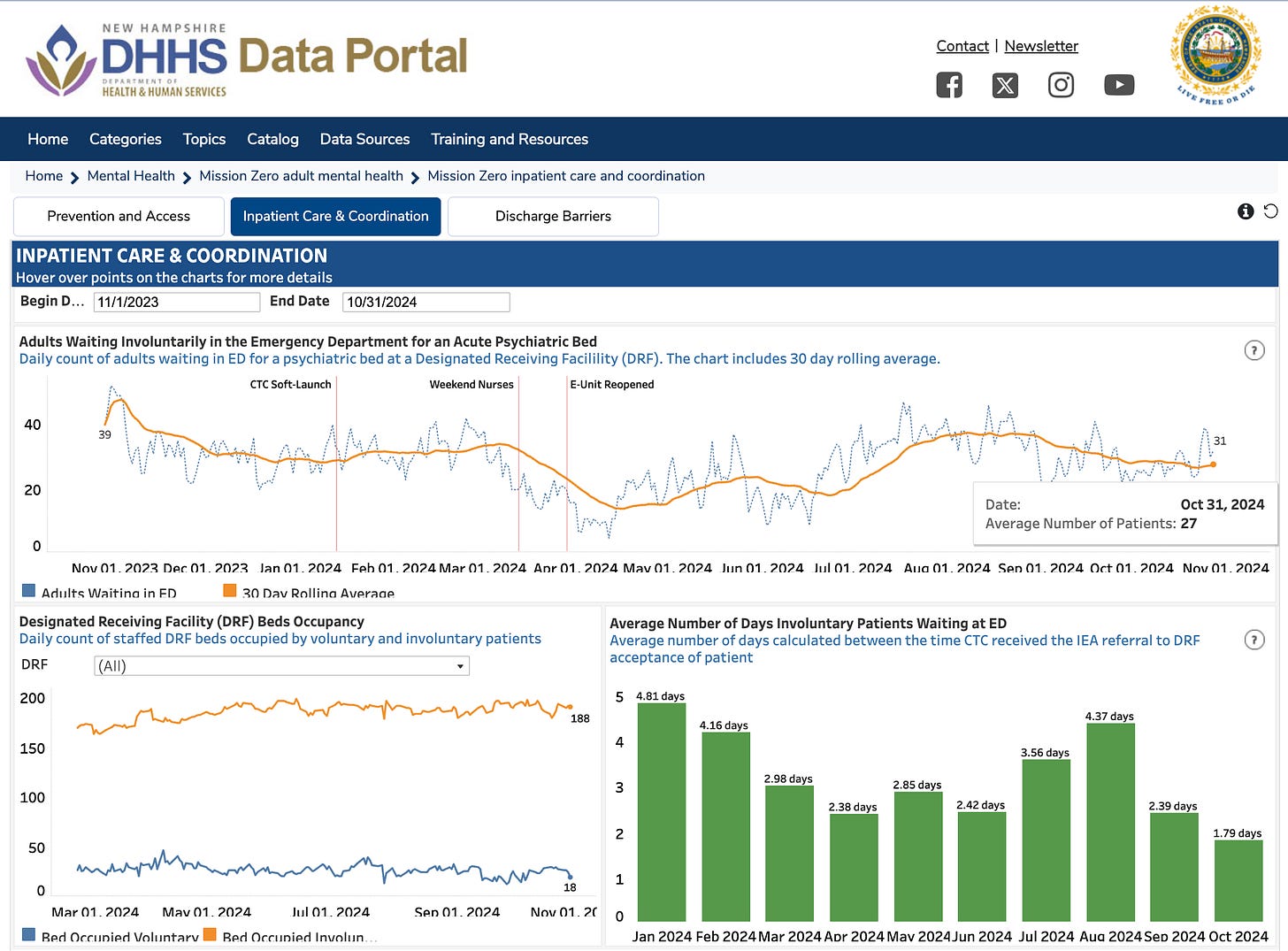
The DHHS Mission Zero dashboard shows that prolonged ED waits were still a problem as of October 2024 (the last month for which data is available on the dashboard). The average number of adults waiting involuntarily in a New Hampshire emergency department for an acute psychiatric bed was 27 per day, not much better than the 2023 average of 31. The average mental health admission waited in an ED for 43 hours in October 2024, far more than the court-ordered limit of six hours.
A project that would have provided a significant expansion of inpatient psychiatric beds in the state - a private 144-bed behavioral health hospital in Londonderry - recently fell through after the town and the health system disagreed on terms. The state had appropriated $15 million of funding for the new hospital’s construction.
Persistent understaffing in New Hampshire’s mental health system, largely as a result of insufficient funding, is a drag on the state’s long-term capacity to deliver psychiatric care. According to the September 2024 interagency report titled Solving the NH Behavioral Health Workforce Crisis, “Workforce shortages in New Hampshire’s behavioral healthcare sector have reached alarming levels and have stayed at these levels for nearly a decade. Despite heroic efforts from leaders from all sectors, many individuals in NH who are in clear need of behavioral health support are not getting sufficient help.”
New Hampshire’s community mental health centers have the mission of keeping patients in their communities rather than being admitted for institutional care. As of the report’s writing, there were 334 open CMHC positions statewide, a 12% vacancy rate. Understaffing also continues at New Hampshire Hospital, the state’s largest psychiatric hospital.
According to a recent New Hampshire Bulletin article, community mental health center “leaders say addressing that need cannot be done without overcoming a paralyzing workforce shortage. They say that can’t be done without an annual increase of $26 million to $28 million for salary increases.”
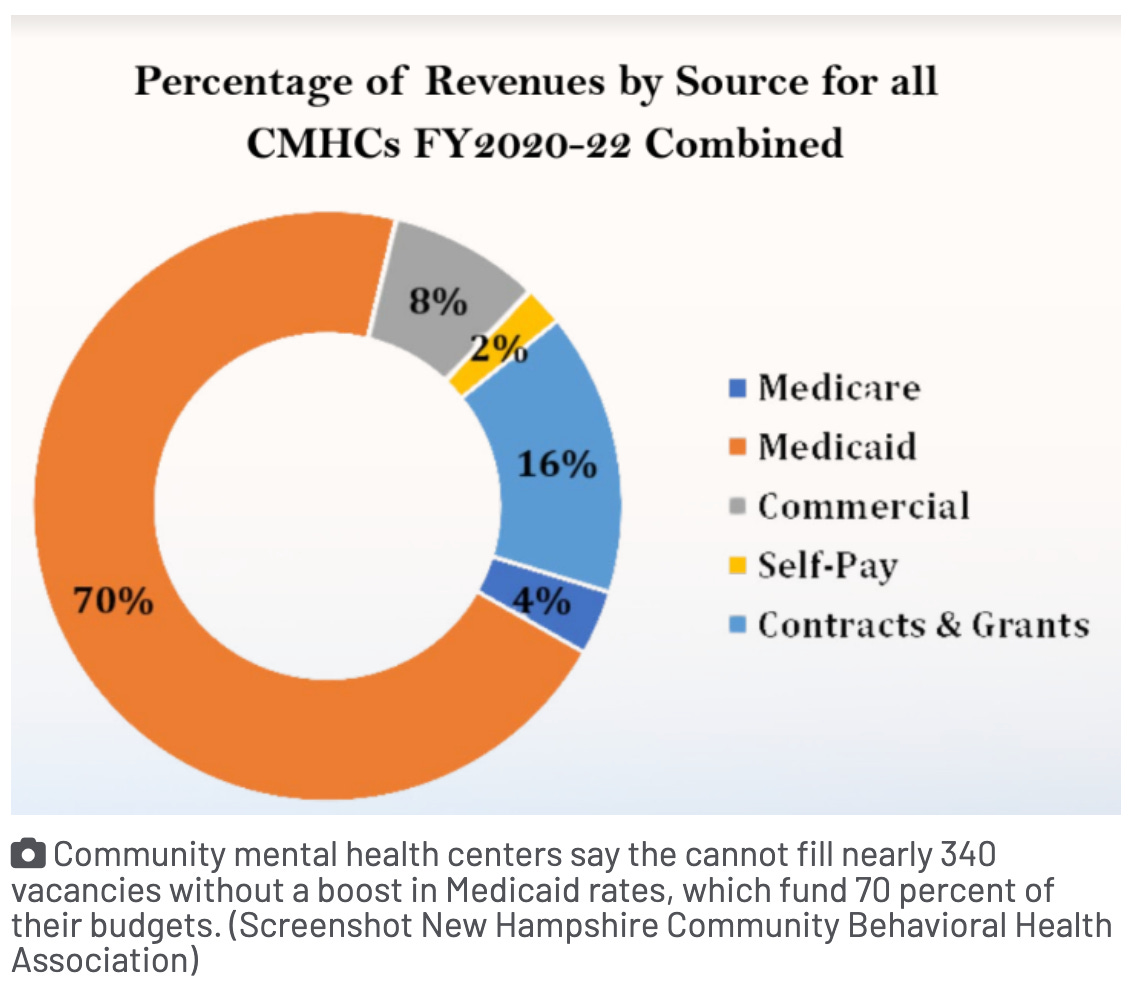
Obtaining enough funding to staff New Hampshire’s mental health system fully will not be simple for the same reason acute psychiatric care is underfunded throughout the country. Mental health care is reimbursed at lower rates than medical and surgical care. Patients with severe mental illness are unlikely to have private insurance, which pays clinicians at higher levels than Medicare or Medicaid. In New Hampshire, only 8% of community mental health center patients have commercial insurance, while 70% are covered by Medicaid.
The bottom line, per Ann-Marie Timmins of the New Hampshire Bulletin: “The state has spent millions to expand mental health treatment in the last two years. Yet those who need it are still waiting.”
Emergency Medicine Workforce Productions is sponsored by Ivy Clinicians - simplifying the emergency medicine job search through transparency.







Psych hospitals don’t want them, ED’s can’t keep them, so out the door they go and the merry goes round and round.