Little-noticed Obamacare clause can save independent EM practices
Also: Physician compensation reports, ChatGPT in the ED, female physicians sued less often, & an emergency physician going to sim-Mars for a year.
Top of the Week
A common explanation for emergency medicine practice consolidation is that small groups get raw deals when negotiating reimbursement rates with large insurance companies. Per this rationale, to tangle with big payors, medical practices should get big too.
US antitrust laws make it illegal for multiple independent medical practices to collectively negotiate reimbursement rates with insurance companies. What if there were a way around those antitrust laws? And what if primary care doctors have already figured it out?
Obamacare - aka Affordable Care Act - holds the secret to physicians negotiating as a big entity while maintaining the benefits of small to medium-sized practices. Based on ACA regulations, the Department of Justice concluded: “the Agencies (FTC and DOJ) will treat joint negotiations with private payers as reasonably necessary to an ACO’s primary purpose of improving health care delivery, and will afford rule of reason treatment to an ACO that meets CMS’s eligibility requirements for, and participates in, the [Medicare] Shared Savings Program and uses the same governance and leadership structures and clinical and administrative processes it uses in the Shared Savings Program to serve patients in commercial markets.”
In other words, independent physician practices can negotiate jointly with private insurers if they are part of an Accountable Care Organization that participates in a Medicare Shared Savings Program. This antitrust exemption applies to fee-for-service parts of the ACO-insurer negotiation as well.
Physician enablement platforms (PEPs), such as Aledade and Privia, have sprung up in response to this market opportunity. Rather than buying medical groups, PEPs bring together independent physician practices, form ACOs, and negotiate improved contract terms with insurers. The PEPs make money through administrative fee structures, while practices increase revenue without giving up independence.
Per Aledade’s founder in a Forbes profile, “‘For physician groups striving to remain independent, it’s all about being able to decide what's best for the patient,’ said Mostashari. ‘If practices are beholden to another set of agendas from an ownership perspective, the duty they owe their employer might be different from the duty they owe patients,’ he said, adding that this conflict often leads to burnout and moral injury for doctors.”
Emergency medicine practices currently face a major hurdle to joining a physician enablement platform. Medicare has not created any emergency medicine Shared Savings Programs. No shared savings means that antitrust rules are enforced for collective bargaining.
The closest entity EM has to a PEP is the Emergency Medicine Business Coalition. EMBC is a “collective of independent democratic emergency medicine practice groups” that enables those practices to “benefit from the same advantages in economies of scale and modern business solutions that larger practice groups enjoy.”
However, due to EM practices’ inability to create ACOs, EMBC’s scale is orders of magnitude smaller than the PEPs. Privia, for example, is valued at $2.8 billion. Meanwhile, EMBC says that their member groups can make a 225% ROI on maximum dues of $10,000.
ACEP is attempting to usher emergency medicine into Medicare’s Shared Savings Program. Every emergency physician knows that the truly expensive decision we make isn’t whether to get a CT scan or an XRay; it’s whether to admit patients to the hospital. Improving admit vs discharge decision-making, as well as the quality of post-ED discharge follow-up processes, has the potential to dramatically decrease Medicare’s spending.
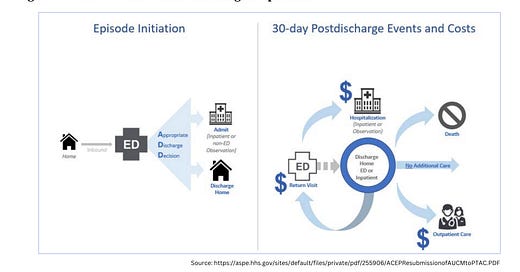
In 2018, ACEP submitted the proposed “Acute Unscheduled Care Model” (AUCM; pronounced “awesome”) to the US Department of Health & Human Services. From that proposal: “Every day, emergency physicians act as gatekeepers to hospitals, making critical decisions about whether the patient should be kept for observation, admitted to the hospital, or discharged. The AUCM model is designed to reflect and reward the important role that emergency physicians play in the health care system. Structured as a bundled payment model, it will improve quality and reduce costs in Medicare by allowing emergency physicians to accept some financial risk for the decisions they make around discharges for certain episodes of acute unscheduled care. It is flexible enough to allow the full spectrum of emergency physicians to participate, should they so choose -- from those with dedicated infrastructure and experience with reporting and meeting quality metrics and taking downside risk, to smaller groups of physicians who do not have as much experience in these areas.”
In October 2019, Alex Azar, the US Secretary of Health & Human Services, gave the AUCM proposal a positive response after passing a key committee vote. However, the pandemic seems to have stalled AUCM’s progress.
For emergency medicine to join with primary care and enter the value-based care era, enacting AUCM (or a similar proposal) is critical. Not only is AUCM a potential win for emergency physicians and practices; it’s also key to improving how acute patient care is delivered in the US.
Exhibit: Q1 2023 results for Privia Health (physician enablement platform)
EM Practice
Medscape’s 2023 Emergency Physician Compensation Report. Sadly, EM is at the bottom of the list when physicians were asked, “Would you choose medicine again?”
Opinion: “We Shouldn't Carry the Full Weight of Responsibility for Our Own Workplace Safety”. “If the federal government requires that all patients be seen, then the government must assume some responsibility for the frontline staff who see them.”
An emergency physician on how ChatGPT and AI can transform healthcare.
House of Medicine
International medical graduate physicians can now practice in Tennessee without completing a US residency program.
Optum and UnitedHealthcare continue squeezing physicians. Arm & a Leg Podcast episode about its new “Payday loan” scheme.
2023 MGMA physician compensation survey: no specialty’s average compensation kept up with inflation.
Post-pandemic Medicaid redeterminations are causing many to lose health insurance. In April, 250,000 Floridians lost their Medicaid benefits.
Per an AMA survey, female physicians are sued less frequently than their male peers. “Research has shown that female physicians ask their patients more psychosocial questions and spend 10% more time with them. One study further found that women doctors provide more preventive care and give more counseling than men. They also score higher on empathy scales, use more egalitarian language, and use less jargon in patient interactions. Yet where it really adds up in terms of patient satisfaction as well as economically is in hospital clinical outcomes. Patients of women hospitalists generally achieve lower readmission and mortality rates than patients of male doctors.”
Hospitals & Health Systems
Craziest business of healthcare story of the week. This one includes private equity scammers, greedy hospital owners, Medicare and real estate fraud, physicians plotting international murder schemes, and so much more.
Minnesota’s legislature attempted to cut healthcare spending. Mayo Clinic had other ideas. Guess who won?
Ascension posted an operating loss of $1.4 billion in Q1 2023. Cleveland Clinic’s operating income in Q1 was $32.3 million.
Kaiser Permanente is giving Denver Health $10 million to help the safety net system stay afloat.
Nursing & Allied Health
Cook County healthcare workers protest over their wages and working conditions.
The Dispo
An emergency physician joins a team simulating living on Mars - for a year.