How big are emergency medicine’s bigs?
Also: Boarding stories, renewing our EM vows, 27-hour PCP work-days, and docGPT’s AI for physicians.
Top of the Week
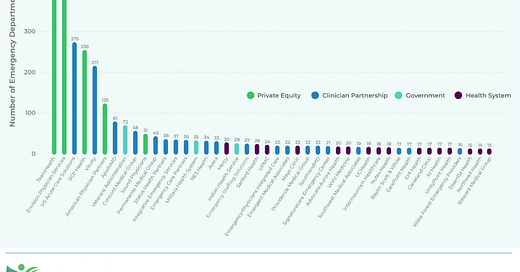
Ivy Clinicians, which is the first to connect every US emergency department with its emergency medicine practice, released its aggregated data this week. Check it out via this link.
Key takeaways from the 2023 State of the Emergency Medicine Employer Market report:
Consolidation has led to 44 emergency medicine employers staffing 15 or more EDs in the US.
Private equity-owned firms manage the clinicians at 24.6% of US EDs, 21.1% of EM residency teaching sites, 17.8% of trauma center EDs, and 28.1% of freestanding EDs.
In aggregate, private equity-owned firms staff less economically desirable EDs than do emergency clinician partnerships. Private equity-owned firms’ staffed EDs are in lower-income, higher uninsurance, and more rural counties.
The US has 676 freestanding EDs. This number is likely to increase more rapidly than the number of hospital-based EDs.
Of employers with 15 or more EDs under management, Northwell Health staffs counties with the highest average per capita income, while SouthlandMD’s facilities are in the lowest average income areas.
EM Practice
Kaiser Health News and NPR published a strongly worded article about increased ratios of PAs & NPs to doctors within emergency medicine groups - especially practices owned by private equity. Per the article, “This staffing strategy has permeated hospitals, and particularly emergency rooms, that seek to reduce their top expense: physician labor. While diagnosing and treating patients was once doctors' domain, they are increasingly being replaced by nurse practitioners and physician assistants, collectively known as ‘midlevel practitioners,’ who can perform many of the same duties and generate much of the same revenue for less than half the pay.”
ACEP has shared over 100 stories from emergency physicians about the challenges of ED boarding. “While the consequences of boarding are felt in the emergency department, the challenges are systemic and there is no single solution. ACEP is leading the call for the White House to convene a summit of healthcare leaders. Collective action is urgent and necessary to help emergency physicians address this crisis and save lives.”
Per this Health Affairs study, there is much variability in rates of mental health ED visits by Medicaid enrollees. Ohio, Nevada, and Iowa have the highest ED visit rates, while Colorado and West Virginia have the lowest rates. Must be something in the mountain air.
A former physician at Jefferson County Health Center has filed a lawsuit alleging that he was wrongfully terminated because of complaints he made about patient safety issues at the health center. “One of those dealt with hospital policy that required emergency room physicians to be responsible for both emergency department patients and general hospital patients.”
Inspiring story of a pediatric emergency physician who, after resuscitating a patient at a wedding along with her husband, “‘renewed my vows’ to the emergency room.”
House of Medicine
After a second loss in federal courts, the US Department of Health & Human Services has temporarily halted the surprise billing resolution (IDR) process. For a podcast explaining the intricacies of the IDR process, check out Ed Gaines’ Zotec Answers.
NY Times: “According to Medical Guidelines, Your Doctor Needs a 27-Hour Workday”.
Biden’s ban on noncompetes could “have big implications on healthcare.” Noncompetes have been shown to decrease wages.
Hospitals & Health Systems
Rural hospitals continue to close, leaving rural patients with fewer care options. “Just because someone lives in a rural area, that shouldn’t mean that they are consigned to second-class healthcare or that their lives aren’t as valuable as someone who lives in an economically advantaged area."
Ascension Health’s operational struggles have gotten the attention of Senator Tammy Baldwin. (Thx to Dr. Arthur Smolensky for the tip.)
Kaiser Permanente posted a $4.5b net loss in 2022.
A Washington Post op-ed argued that health systems should shift some of their marketing budgets toward hiring more staff. “According to a report in the Journal of the American Medical Association, between 2004 and 2016, direct-to-consumer advertising by hospitals and healthcare systems jumped 74 percent to $1.4 billion per year… If spending on advertisements is nonnegotiable but hiring enough nurses to save patients’ lives isn’t, who is our healthcare system truly serving?”
Nursing & Allied Health
Nursing licensure compacts between states have simplified the nursing credentialing process.
Dartmouth’s “Shark Tank for nurses” inspires staff to come up with creative ideas to improve care delivery.
The Dispo
Doximity has released a version of ChatGPT tailored to physicians, called docsGPT.