How AAEM can win on Corporate Practice of Medicine, even without Envision
Also: Fear in the ED, massive investments in primary care, hospital price transparency, and decreasing rates of nurse turnover.
Top of the Week
Envision is barreling toward bankruptcy.
From AAEM’s perspective, this may sound like good news in their longstanding fight against the corporate practice of emergency medicine. However, bankruptcy usually leads to the termination of civil lawsuits against the bankrupt company. Envision’s bankruptcy would likely halt AAEM’s lawsuit claiming that Envision violated California’s Corporate Practice of Medicine laws.
AAEM can still win on corporate practice of medicine, even without Envision. The key would be uniting the organized House of EM.
The ACEP Council in October 2022 passed a resolution titled, “Policy Statement on the Corporate Practice of Medicine”, submitted by Drs. Pattavina, McNamara, and Dreifuss. This resolution instructs ACEP to “Adopt a policy statement on the corporate practice of medicine based on the California Medical Board’s guidance.”
Important section of the 2022 ACEP Council resolution on CPOM:
—
The following “business” or “management” decisions and activities, resulting in control over the physician’s practice of medicine, should be made by a licensed physician and not by an unlicensed person or entity:
Ownership is an indicator of control of a patient’s medical records, including determining the contents thereof, and should be retained by a licensed physician.
Selection, hiring/firing (as it relates to clinical competency or proficiency) of physicians, allied health staff and medical assistants.
Setting the parameters under which the physician will enter into contractual relationships with third-party payers.
Decisions regarding coding and billing procedures for patient care services.
Approving of the selection of medical equipment and medical supplies for the medical practice.
The types of decisions and activities described above cannot be delegated to an unlicensed person, including (for example) management service organizations. While a physician may consult with unlicensed persons in making the “business” or “management” decisions described above, the physician must retain the ultimate responsibility for, or approval of, those decisions.
The following types of medical practice ownership and operating structures also are prohibited:
Non-physicians owning or operating a business that offers patient evaluation, diagnosis, care, or treatment.
Management service organizations arranging for or providing medical services rather than only providing administrative staff and services for a physician’s medical practice (non-physician exercising controls over a physician’s medical practice, even where physicians own and operate the business).
In the examples above, non-physicians would be engaged in the unlicensed practice of medicine, and the physician may be aiding and abetting the unlicensed practice of medicine.
—
It may be tempting to dismiss this passed ACEP resolution as yet more tilting at windmills from academics trying to return EM to an imaginary time when business interests were separate from the practice of medicine. However, there is reason to believe that an ACEP policy based on this CPOM resolution would actually have teeth. The reason: the “friendly physician”.
Thirty-four states have enacted the Corporate Practice of Medicine Doctrine. In CPOM Doctrine states, for a non-physician-owned entity to own a medical practice, it must enter into an arrangement with a physician who remains the legal owner of the practice. In exchange, that “friendly physician” agrees to transfer nearly all revenue and control of the practice to the purchasing corporation.
If both AAEM and ACEP have strong policies against the corporate practice of medicine, they still would not have direct recourse against the purchasing corporations (eg: KKR or Blackstone). Instead, they could target “friendly physicians”. Removing the physician figurehead from the corporate-owned medical practice structure would collapse the firm like pulling out a foundational block in a Jenga game.
Such physicians could be censured by ACEP and AAEM, which would send a strong message to other physicians and hospitals that corporate ownership of EM practices will not be tolerated. Hospitals would be less likely to contract such a group and physicians would be less likely to place themselves in a position to be censured by their specialty’s organizing bodies.
If ACEP was willing to censure Peter Rosen, one of the specialty’s founders and greatest advocates, I would not bet against the College to uphold a future CPOM policy through the censure process.
EM Practice
Thought-provoking commentary from an emergency medicine resident in Annals about fear in the ED.
ACEP’s ED Workplace Safety Checklist.
A surprisingly constructive discussion of solutions to EM burnout in Facebook’s EM DOCS group (password required).
If you ever doubted that emergency medicine is complex, check out the “Model of Clinical Practice” from Annals.
House of Medicine
From a JAMA study of 81755 students taking the MCAT: “American Indian or Alaska Native, Black, and Hispanic examinees had lower parental educational levels and greater financial and educational barriers (eg, outstanding premedical loans) than White examinees. These barriers were associated with lower likelihood of applying to and matriculating at medical school and largely accounted for racial and ethnic differences in application and matriculation.” NPR story about this study.
Health Affairs examines why Amazon, CVS, and Walgreens are spending so much money to get into the primary care business.
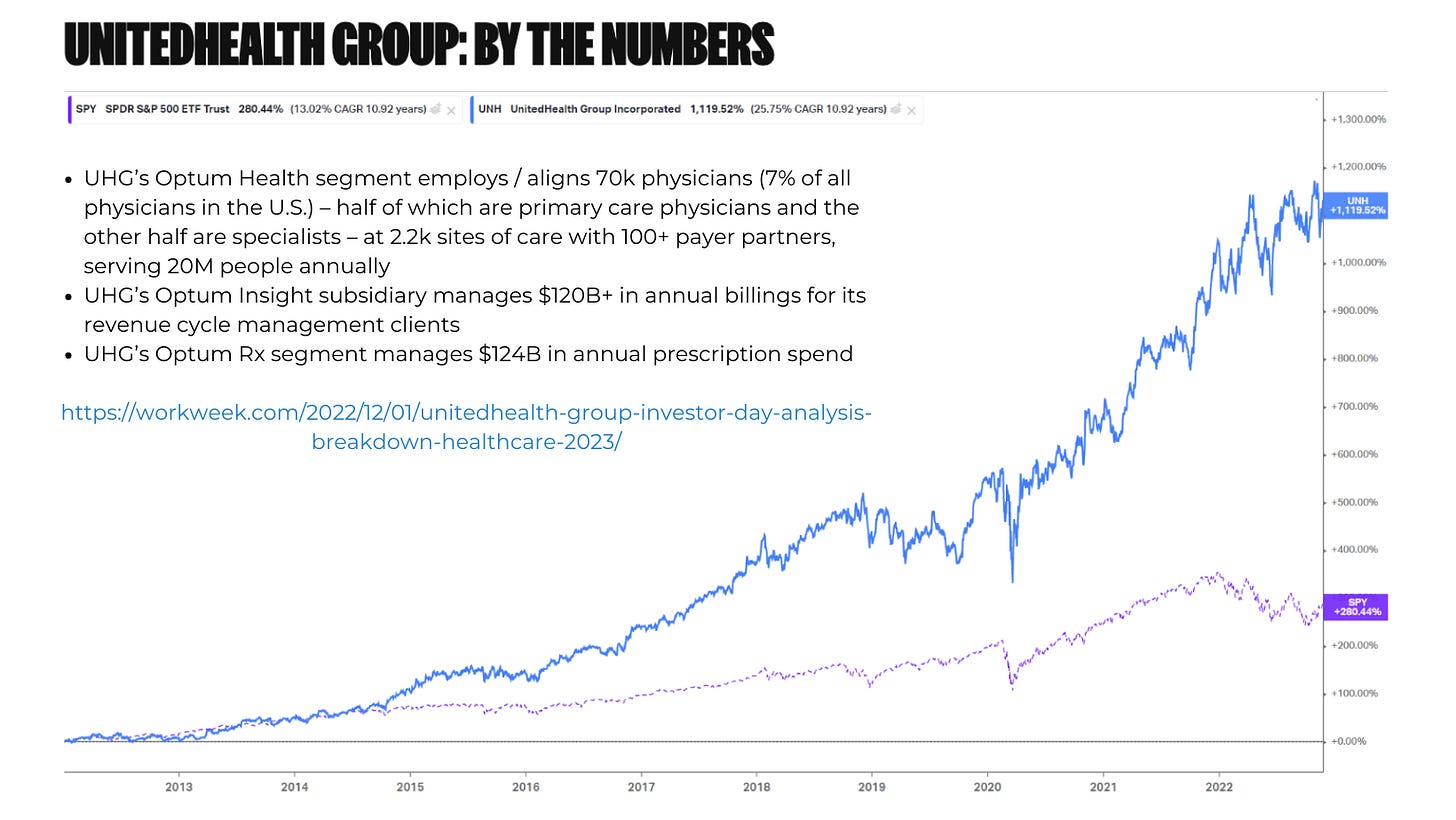
UnitedHealth is doing very well, largely due to the growth of Optum and Medicare Advantage.
HCA is working with Augmedix to automagically transcribe ED patient visits into the EMR. AI is coming for EM documentation.
Letting insurers run hospices might not be great for patient outcomes.
Discussion of rural physician shortages.
Hospitals & Health Systems
Hospital price transparency is actually progressing, per Turquoise Health.
Health systems are increasing their investments in venture capital, an important funding source for physician innovators.
AHA report on how hospital expenses are rising much faster than revenues.
Nursing & Allied Health
Study: “Examining the Impact of the COVID-19 Pandemic on Burnout and Stress Among U.S. Nurses”. …high proportions reported feeling emotionally drained (50.8%), used up (56.4%), fatigued (49.7%), burned out (45.1%), or at the end of their rope (29.4%) "a few times a week" or "every day."
800,000 nurses say they intend to leave the nursing workforce by 2027. (full article link)
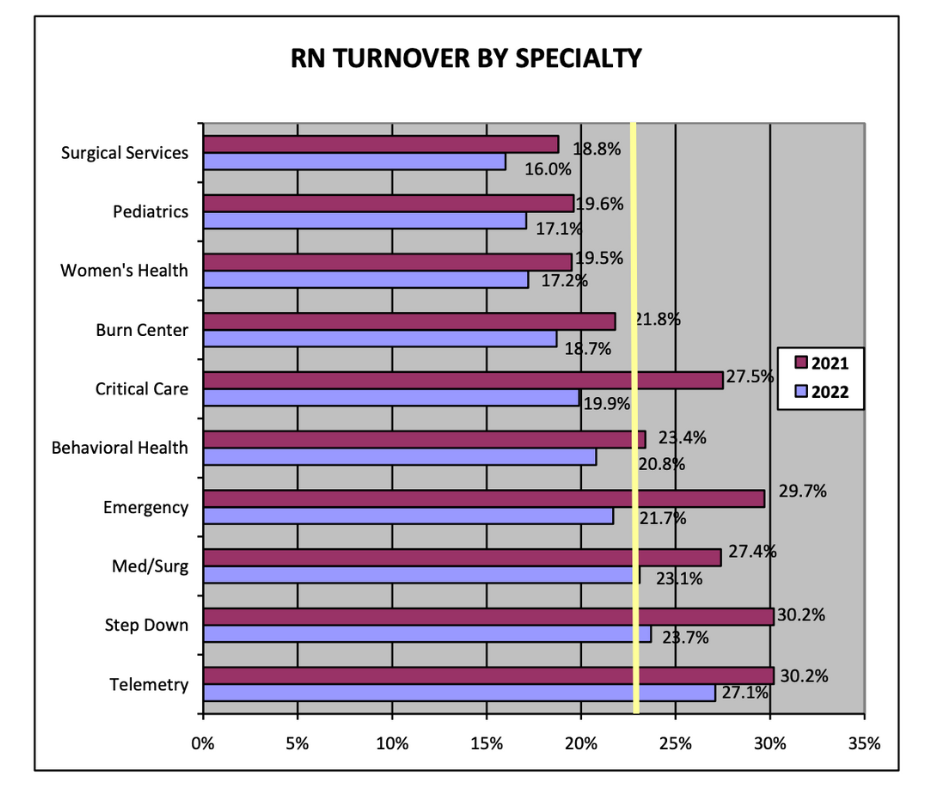
2023 NSI National Health Care Retention and RN Staffing Report. Heightened turnover rates are driving hospitals to use more healthcare staffing tech.
The Dispo
Very cool to see a profile of a retired emergency physician in the Wall Street Journal. A nice reminder that emergency physicians are still bad-ass (BAFERDs).