Emergency Physician Compensation is (somewhat) Related to Supply & Demand
An analysis of Ivy Clinicians' salary survey for attending emergency physicians shows that compensation is higher in poorer counties and in mid-sized communities.
That emergency physician compensation is partly determined by supply-demand dynamics is a truism of the emergency medicine job market. But is it true?
Ivy Clinicians’ attending emergency physician salary survey received 947 entries between January 1, 2023 and November 21, 2024. This enabled us to explore the relationship between a U.S. county’s desirability for emergency physicians to live in - using the county’s wealth & urbanity as proxies - and median emergency physician salaries in those areas.
Emergency Physician Compensation per Hour (median) by County-level Per Capita Personal Income
Ivy’s 2023-2024 salary survey analysis showed a negative correlation between a county’s overall wealth and median emergency physician compensation.
Attending emergency physicians who work in counties with per capita incomes greater than $70,000 per person earned approximately $20 less per hour in total compensation than those who live in poorer counties. Emergency physician hourly compensation was $24 per hour greater in the poorest counties (those with per capita incomes less than $50,000 per year) than in the wealthiest counties (average incomes greater than $100,000 per person).
The inverse correlation between emergency physician salaries and community wealth is consistent with the supply-demand hypothesis. As highly educated professionals, most physicians prefer to live in wealthier communities. Extra pay is needed to inspire most physicians to commute to less prosperous communities.
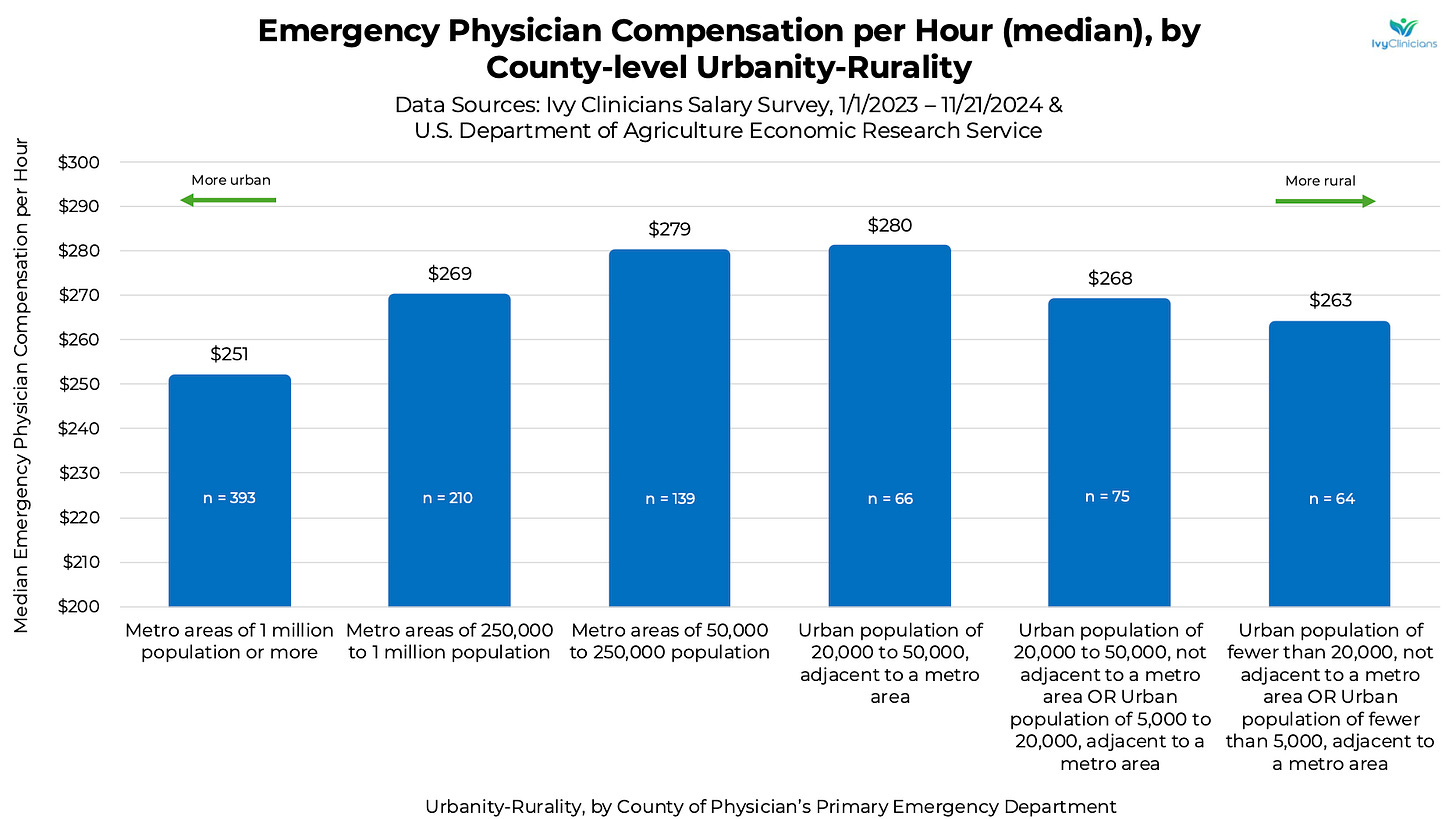
Emergency Physician Compensation per Hour (median) by County-level Urbanity-Rurality
The salary survey data showed a biphasic relationship between urbanity-rurality and emergency physician compensation.
Hourly pay in the most urban counties was approximately $30 lower than compensation in mid-sized communities. However, the inverse was also true. Emergency physicians in most rural counties were paid $17 per hour less on average than in mid-sized communities.
Our hypothesis for lower compensation in the most rural regions is that some rural emergency departments have fewer patients to be seen by the physician. Low-volume EDs may be able to attract some physicians, even at lower pay, because of decreased workloads.
Another potential explanation is that rural emergency departments are more likely to staff physicians who are not residency-trained and board-certified in emergency medicine. Family medicine-trained physicians may be willing to work for lower salaries than board-certified emergency physicians.
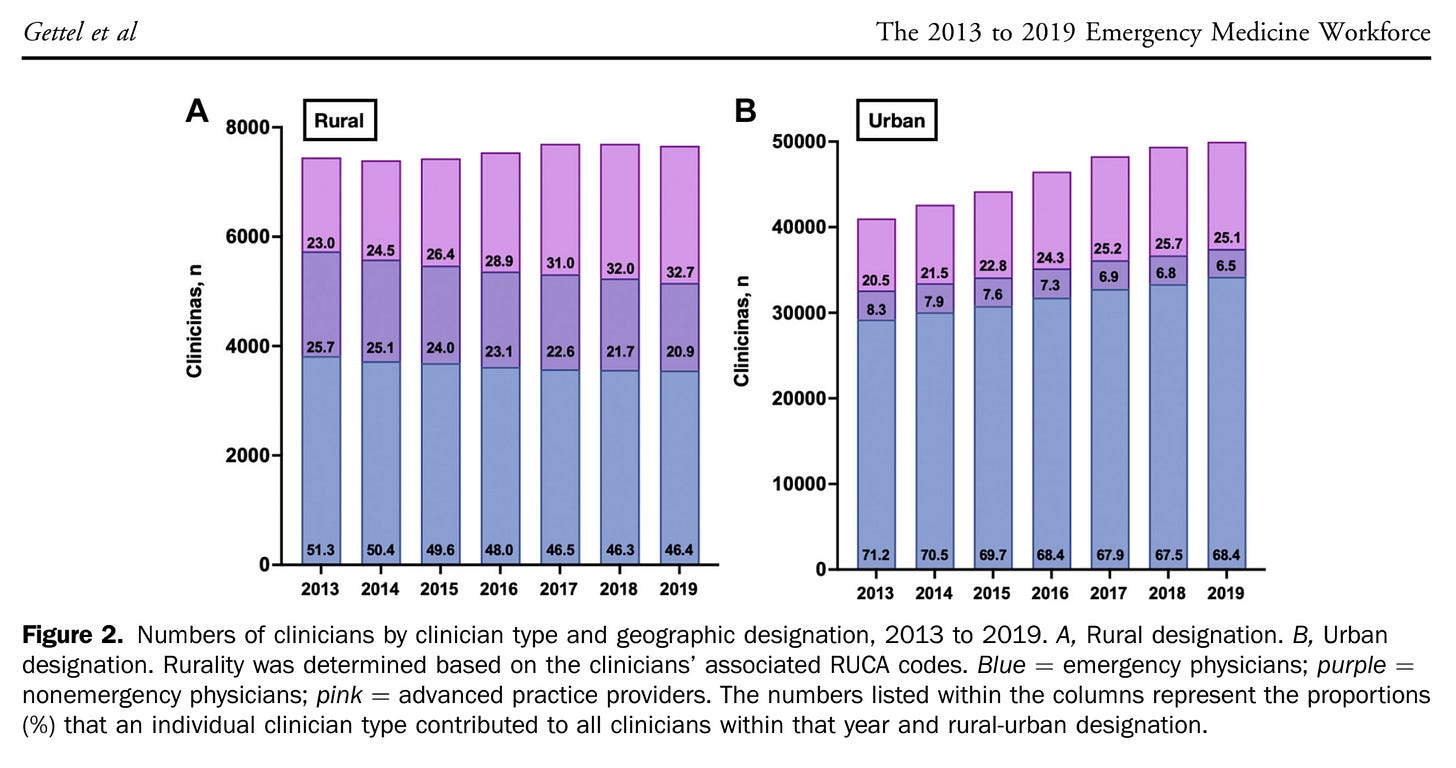
In “The 2013 to 2019 Emergency Medicine Workforce: Clinician Entry and Attrition Across the US Geography,” Gettel et al found that “emergency physicians comprise less than half of the rural emergency medicine workforce, initially representing 51.3% in 2013 and decreasing to 46.4% of all clinicians serving rural designations in 2019.”
The “National Study of the Emergency Physician Workforce, 2020” by Bennett et al. reported that the “population density of emergency physicians in rural areas, especially those who are emergency medicine trained or ABMS emergency medicine board certified, is much lower than in urban areas.”
Notes on Methods
Dates of included salary survey entries: January 1, 2023 through November 21, 2024.
Only attending-level emergency physician entries were included.
Locum tenens and travel physician survey entries were excluded.
Total compensation included hourly salary + bonus compensation + benefits when offered. We estimated the value of benefits to be a 20% addition to the salary. Of the 947 salary entries, 531 were W-2s (employees), 369 were 1099s (independent contractors), and 47 were K-1 (partners). Salary.com’s breakdown of average benefits for emergency physicians in the U.S. is as follows:
Limitations
This analysis is based on physician-entered salary surveys, which have inherent recall bias.
Emergency medicine practice partners were under-represented in the sample. Less than 10% of salary surveys were from self-identified practice partners.
The monetary equivalent of benefits is difficult to quantify in a salary survey. The +20% estimate was generated as a mid-point of the following sources:
The Cost Shifting Economics of United States Emergency Department Professional Services (2016–2019): “For benefits (eg, health care coverage, 401k contribution, etc), we reviewed the Bureau of Labor and Statistics National Compensation Report for service occupations, where benefits in the hospital industry averaged 34% of wages, but used a lower estimate (30%) because ED clinicians, especially physicians, have relatively high hourly rates.”
White Coat Investor: “As a general rule for a physician with an income near the median physician income in the $250,000 range, I would estimate that a typical independent contractor job ought to pay about 10% more to be equal to the typical employee job. But that rule of thumb is worth about what you paid for it since there is so much variation out there.”
https://www.salary.com/research/salary/alternate/emergency-medicine-physician-salary
Data Sources
U.S. Bureau of Economic Analysis Personal Income by County and Metropolitan Area, 2023, released November 14, 2024
U.S. Department of Agriculture Economic Research Service 2023 Rural-Urban Continuum Codes, updated 1/22/2024
Emergency Medicine Workforce Productions is sponsored by Ivy Clinicians - simplifying the emergency medicine job search through transparency.






Great article, it tracks exactly with my experience in rural hospitals, particularly noting that much of rural emergency medicine is done by non-EM boarded docs (and in some cases independent APPs) driving down hourly pay in smaller communities. Also noted is the lower workload, which is likewise correct. The only thing I'd add in rural EDs is the ability to work longer shifts (24-48 hours in some cases) which mitigates longer commutes and lower hourly rates.