Emergency medicine’s Texan brawl with regulators & insurers over the No Surprises Act
Top of the Week
Arbitration rules from the No Surprises Act will determine how much emergency medicine practices get reimbursed for care delivered to privately insured US patients. Not surprisingly, insurers have lobbied for the law to be implemented in their favor.
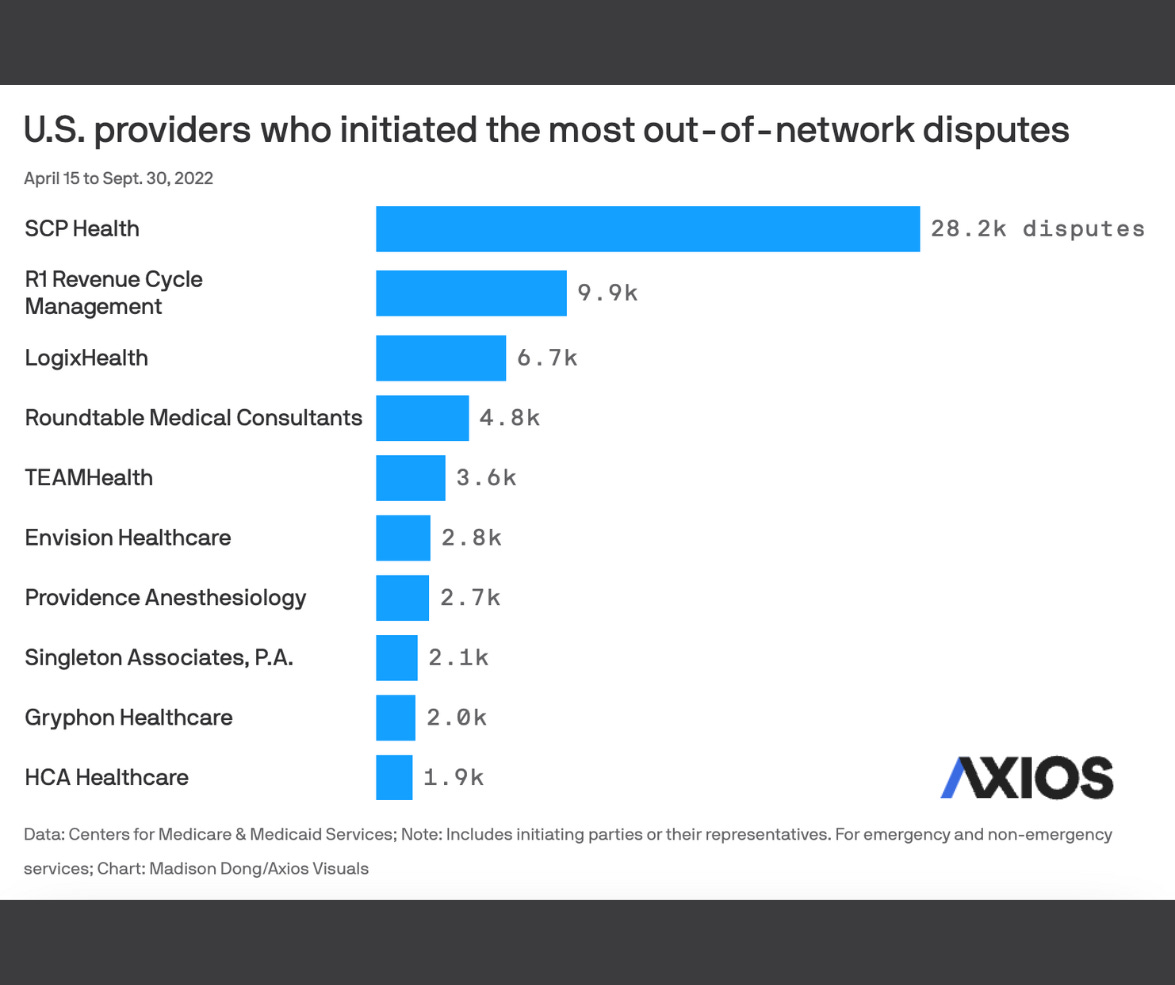
EM practices are fighting back. Per CMS’ Initial Report on the Independent Dispute Resolution (IDR) Process, 81% of submitted arbitration cases were for ED services. Emergency medicine firms disputed 70,071 cases from 4/15/22 to 9/30/22. The arbitration case volume in the IDR’s first five months was higher than CMS projected for the whole year.
SCP Health submitted the largest number of IDR disputes, with 32% (n=28,196). R1 Revenue Cycle Management (11%), LogixHealth (8%), TeamHealth (4%), and Envision (3%), submitted arbitration cases on behalf of emergency clinicians.
Meanwhile, the Texas Medical Association has taken the US Department of Health & Human Services to federal court three times in the last 14 months over IDR regulations. TMA won the first round, then sued again alleging that DHHS did not comply with the initial ruling. TMA’s third lawsuit claims that insurers are using illegal means to deflate the “qualifying payment amount (QPA)”, which arbitrators use to help decide appropriate reimbursement rates. TMA’s suits have been filed in the Fifth Circuit, which has a reputation for being the US’ most conservative set of federal courts.
EM Practice
The TEAMM Project is ramping up miscarriage management training for emergency clinicians across the country.
The New York Times looks into the effect of reimbursing hospitals less for pediatric than for adult care.
House of Medicine
Per a JAMA study of US healthcare worker unionization, “Reported union membership or coverage was significantly associated with higher weekly earnings and better noncash benefits but greater number of weekly work hours.”
The former Chief of Pediatrics at Harborview: Our fraying health care system is reaching a breaking point (in the Seattle Times).
Advisory Board’s 16 Things Healthcare CEOs Need to Know in 2023.
See how much the US spent on healthcare, by service type, 1960-2021. (from KFF)
Hospitals & Health Systems
Health systems have been consolidating rapidly. Much depends on how the Federal Trade Commission regulates these mergers in the coming years.
Forbes’ list of best hospitals to work for, by state.
Hospital margin projections for 2023 are weak, largely due to anticipated high labor costs.
Nursing & Allied Health
Travel nursing pay is dropping, as post-pandemic demand normalizes.
The Dispo
The inspiring story of the reunion of a Marine physician and his trauma patient from the Vietnam War, brought together by a photo.