Black and Hispanic medical students graduate with more debt than White and Asian students.
Also: EM residency application numbers are far lower than pre-pandemic, the feds lose to provider groups in court over the No Surprises Act, and the “difference between mostly dead and all dead."
Top of the Week
Of practicing emergency physicians in the US, only 4.9% identify as Black and 6.1% are Hispanic, as compared with 13.6% and 18.9% respectively for the population as a whole.
The US medical training process presents financial barriers to increasing the number of Black and Hispanic physicians. These communities have fewer savings to support years of uncompensated study. In a 2019 Federal Reserve survey, Black median family wealth ($24,100) was less than 15% of White median family wealth ($188,200). Hispanic median family wealth in the US was $36,100.
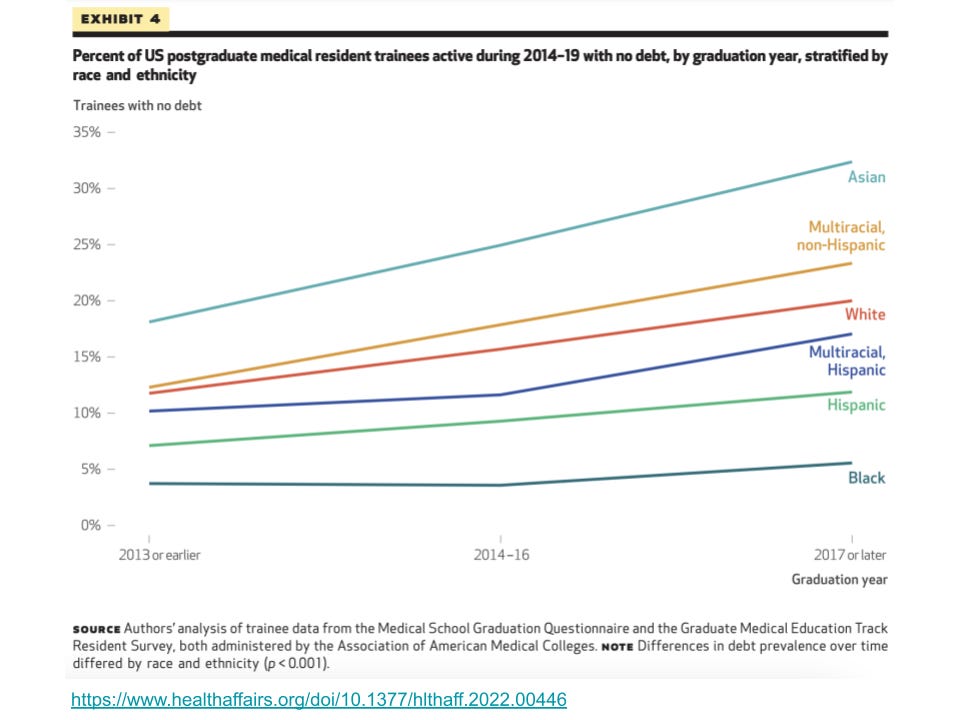
A study in this month’s Health Affairs, “Differences in Debt Among Postgraduate Medical Residents by Self-Designated Race And Ethnicity, 2014-2019”, shows that Black and Hispanic medical students graduate with significantly more debt than White and Asian students in the US. The authors found that “all types of debt were significantly more common among trainees from populations underrepresented in medicine compared with White and Asian trainees (p < 0.001). Black trainees were consistently most likely to have debt, including 95.5 percent with any debt (95% CI: 94.9, 96.0), and a majority of Black trainees had debt from premedical education loans (59.9 percent; 95% CI: 58.7, 61.1) and consumer debt (50.4 percent; 95% CI: 48.5, 52.3).”
Excessive financial barriers to entry into the profession of medicine not only lead to less diversity but also unnecessarily block talented students from choosing to become physicians. For brilliant scientifically oriented students with minimal family wealth, it is financially understandable for them to choose careers such as software engineering over medicine.
The paper concludes: “Given the country’s interest in fostering a diverse health care workforce, addressing student loan debt may make matriculation to medical school, and success throughout medical training, more attainable for a diverse group of Americans.”
Note: click here for Health Affairs’ podcast episode discussing this study.
EM Practice
Dr. Thomas Cook discusses the decrease in medical students applying for the emergency medicine match as compared with before the pandemic (while new EM residencies continue to open).
Provider groups won a federal court case about the No Surprises Act. The decision kicks regulatory decisions over the dispute resolution process back to the Health and Human Services Department. An EDPMA survey shows the many ways the IDR is being gamed by insurance companies.
House of Medicine
Per Today’s Hospitalist, “Average pay for hospitalist APPs, according to our survey, comes in at just over $150,000.”
CVS bought value-based primary care provider Oak Street Health for $10.6 billion.
Private equity healthcare deals slowed during 2022, per Pitchbook. Cardiology practices are the “new darling of private equity investment.”
New York Times Op-Ed: “Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System.”
Powerful JAMA opinion article by Dr. Don Berwick about the impact of greed on US healthcare. “Greed harms the cultures of compassion and professionalism that are bedrock to healing care. Healthcare executives and board members who know better nonetheless feel compelled to play the games of pricing, acquisition, and revenue maximization that others do. Professionals find themselves trapped in record keeping, coding behaviors, and productivity imperatives that belie the reasons many went into health care in the first place. ‘Moral injury’ is the harvest, with demoralization and disengagement to follow.”
Hospitals & Health Systems
Maryland has the longest ED wait times in the US.
Deep dive into HCA Healthcare’s finances and what they mean for the hospital market.
Hospitals are defending themselves from ransomware (Tallahassee Memorial) and violent patients (Duke).
Nursing & Allied Health
Though overall US job growth was strong in 2022, employment in hospitals and post-acute residential care are still below 2019 levels. Employers are responding with increased compensation.
Nurses in Watertown, NY picket over understaffing.
Average hourly salary for RNs, by state.
The Dispo
An Iowa patient was found by a funeral home to be breathing inside a body bag. Princess Bride reminder: “There's a big difference between mostly dead and all dead. Mostly dead is slightly alive.”