A Chance to Fix America’s Worst Business Model (Emergency Mental Health)
Also: Practice buy-ins, hospitals jacking up facility fees, healthcare's everything merger = “vertical integration”, and countries competing for nurses.
Top of the Week
Can you imagine a worse business model than acute mental healthcare in the United States? The current system for managing patients with acute suicidality and psychosis harms nearly all of its key stakeholders.
Acute behavioral health patients who most need care are kept in prison-like conditions for days without proper treatment. Clinicians caring for them are mismatched with patients’ needs and are dramatically under-compensated for the care provided. Hospitals, most of which theoretically do not provide psychiatric services, are compelled by the government to deliver those services at a steep financial loss.
(Caveat: private insurers benefit from the current acute psychiatric care system. Because they always win. However, most ED psychiatric patients don’t have commercial insurance.)
Three recent developments have opened a window of opportunity to reshape acute care psychiatry: 1) a federal court ruling that New Hampshire’s acute mental health ED boarding is unconstitutional; 2) the proliferation of EmPATH units; 3) increased availability of US government funding for mental health. Let’s dig into each element.
Four anonymous patients, twenty New Hampshire hospitals, and the New Hampshire Hospital Association sued the New Hampshire Department of Health and Human Services, claiming that prolonged ED boarding - four weeks in the case of one of the plaintiffs - was unconstitutional under the Fourth Amendment. On February 23, 2023, Judge Landya McCafferty of the Federal District Court, ruled for the plaintiffs. This led to a multi-stakeholder agreement, “Mission Zero”, to ensure all ED psychiatric patients in New Hampshire depart within six hours of their involuntary commitments, by May 2024.
The case’s details are worth delving into since each state has different acute mental health treatment laws. As one analysis said, “We are running 50 different experiments, with no two states taking the same approach. As a result, whether a person receives timely, appropriate treatment for an acute psychiatric crisis or chronic psychiatric disease is almost entirely dependent on what state that person is in when the crisis arises.” Though this case was decided in federal court, the ruling was a Constitutional evaluation of New Hampshire state laws. Harnessing the ruling in your state will require an understanding of the way state laws overlap.
The Fourth Amendment protects against unreasonable seizures of property by the government. The full text: “The right of the people to be secure in their persons, houses, papers, and effects, against unreasonable searches and seizures, shall not be violated, and no Warrants shall issue, but upon probable cause, supported by Oath or affirmation, and particularly describing the place to be searched, and the persons or things to be seized.”
In New Hampshire, involuntarily committed psychiatric (IEA) patients become “the Commissioner’s patient in the state’s mental health services system.” Once the IEA is legally served, primary responsibility for a patient’s care changes from the hospital to the state.
The state argued that the physicians and hospitals made independent decisions to commit the patients, so the patients were the hospitals’ responsibility. The judge responded, “The Commissioner argues, as she has previously, that her boarding practice does not constitute state action because hospital staff, not state actors, complete the IEA certificates based on their voluntary and discretionary decisions. The Commissioner is mistaken… The New Hampshire Supreme Court held that the approved medical providers who perform those actions are acting as part of the state’s mental health services system.”
The ruling includes pages of examples of prolonged ED boarding of IEA patients. Involuntary boarding led to significant harm to the hospitals’ operations. Simply, “the Commissioner is seizing the Hospitals’ emergency departments by boarding her patients there without the permission of the Hospitals.”
The plaintiffs also had to show that the seizures were unreasonable to meet the Fourth Amendment threshold. In siding against the state, the judge clarified that New Hampshire has “no governmental interest in failing to receive IEA-certified patients in designated receiving facilities.”
In contrast, hospital emergency departments are legally required to properly care for all arriving patients. “The Hospitals’ interest is not just a private possessory property interest; the Hospitals also have a legal obligation to operate functioning and available emergency departments.” As the seizure is not a state obligation and violates the state-determined obligations of the ED, the seizure of hospital resources is deemed unreasonable.
The case’s summary statement: “The Commissioner has violated and continues to violate the Hospitals’ Fourth Amendment right (made applicable to the states through the Fourteenth Amendment) to be free from unreasonable seizures of their emergency departments through her conduct, policies, and practices that fail to allow IEA-certified patients to be immediately transported from the Hospitals’ emergency departments to designated receiving facilities.”
A favorable Constitutional ruling is helpful, but does not solve the practical problem of where acute psychiatric patients should be cared for. Per the Treatment Advocacy Center, “By early 2016, the practice of closing state mental hospitals, often called ‘deinstitutionalization,’ had eliminated more than 96% of the last-resort beds that existed in the mid-1950s; after a brief period of expansion in the 1990s, private hospitals, too, are shrinking their psychiatric inpatient capacity.” The demand for acute care psychiatry has increased as care supply has collapsed.
Enter EmPATH (emergency psychiatric assessment, treatment, and healing). EmPATH was created by Dr. Scott Zeller who now works with Vituity, though both the EmPATH name and model are non-proprietary. Per Zeller, he was advised to copyright the term EmPath but decided not to, so other providers could more easily adopt it.
A recent New Yorker profile of EmPATH described the units as, “instead of leaving patients to languish in an emergency room, caregivers offer them a calm communal environment where they can receive a comprehensive evaluation, start therapy, and, if needed, receive medication. Most patients stay for a day or two; the vast majority are discharged back home, instead of going on to a psychiatric facility.” A 2022 study in Academic Emergency Medicine showed that introducing an EmPATH unit decreased psychiatric admissions by half and ED boarding time by two-thirds.
The main hurdle to the wider adoption of EmPATH is financial. Though the units save money for the system while providing high-quality care, they lose money within the current reimbursement structure. Per a Mental Health America report, “The current rate-setting processes are specifically designed to disadvantage behavioral health because of who sets the rates and what they consider. The market reimbursement rate for out-of-network behavioral health care is so much higher than in-network rates in Medicaid, Medicare, and private insurance, showing that the current reimbursement rate-setting process is failing.”
The market is unlikely to solve the acute mental health funding shortfall. However, more government funding is available now than in past decades. The 2022 firearms bill passed by Congress actually was “kind of a gun safety bill wrapped in a mental health bill,” said Jeffrey Swanson, a psychiatry professor at the Duke University School of Medicine who studies the intersection of gun violence and mental illness. The bill appropriated $13 billion for mental health initiatives.
States, including New Hampshire, have been ramping up mental health spending. Governor Chris Sonunu’s main critique of the mental health federal court case was that the New Hampshire government was already prepared to spend large sums on mental health.
With the increase in government funding for acute mental health, a new model of care that efficiently provides high-quality acute psychiatric care outside of the ED, and a federal court holding that prolonged ED behavioral health boarding is unconstitutional, the time is right for the House of Emergency Medicine to advocate for state-level reforms. Our past failed attempts to improve the system are no excuse for missing this important opportunity.
EM Practice
Per KFF data, ED facility fees have grown more than twice as fast as emergency physician fees over the last two decades. "Emergency department facility fees increased 531% from 2004 to 2021 (from $113 in 2004 to $713 in 2021) and 112% in the past decade (from $337 in 2012 to $713 in 2021). Facility and professional fees were comparable in 2004, but by 2021 the average facility evaluation and management claim was more than twice as expensive as the average professional evaluation and management claim."
In a heartfelt and thoughtful article, Dr. Yang Wang discusses why he still believes in the value of emergency medicine practice. One paragraph: “I know there are important, justified reasons why good doctors are leaving EM. Metrics suck. Non-physicians running hospitals and dictating how to treat patients suck. Insurance companies playing payment denial games and lobbying on state and federal levels to lower reimbursement suck. Outside consulting firms telling us to do our job better with fewer staff sucks. But right now, in my own personal recruitment experience this year, and in the social media bubble I’m swimming in, it feels like EM docs have shifted priorities from finding joy in the hard work of treating sick human beings, from wanting to use all our skills to our utmost to instead looking for the easiest work for the best pay.”
Insightful Reddit discussion of emergency medicine private practice buy-ins.
House of Medicine
The feds are (again) pushing for insurance parity between mental health and physical health.
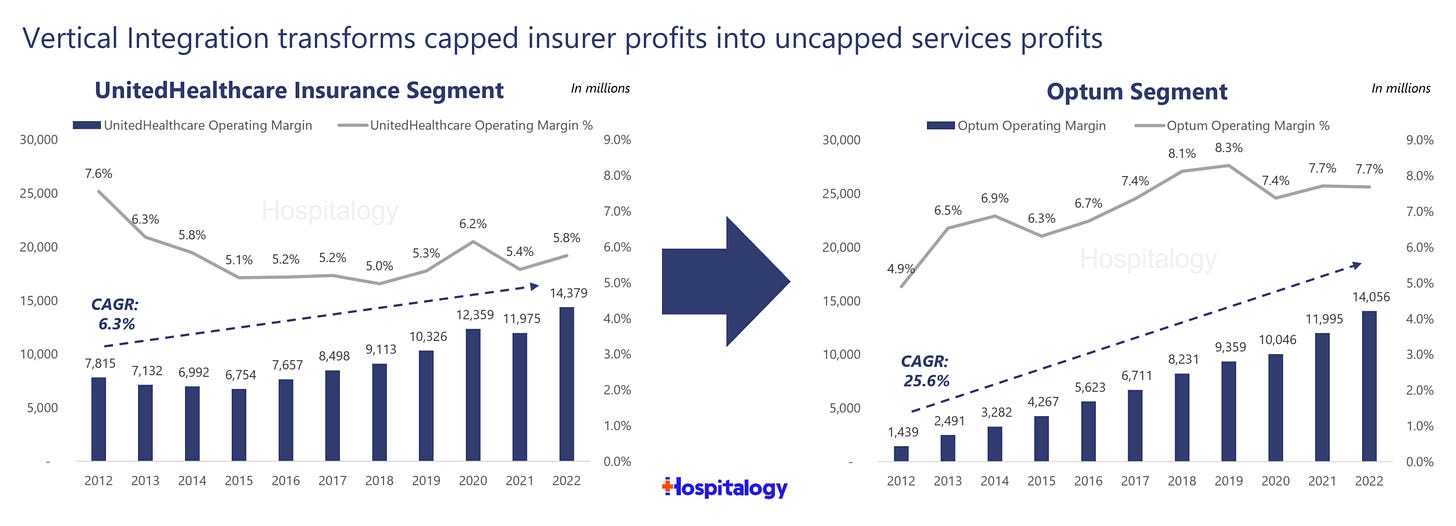
A solid summary of “vertical integration” among insurers, hospital systems, and pharmacies.
Hospitals & Health Systems
In the Wall Street Journal, Louisiana’s former governor Bobby Jindal calls hospitals’ outpatient billing practices “dishonest”.
Sanford and Fairview Health called off their proposed merger in a sign of increased antitrust enforcement. Check out the updated FTC-DOJ merger guidelines.
Nearly half of Mississippi’s hospitals are at risk of closure. The underfunding of rural hospitals is a national problem, though worse in states that have not expanded Medicaid.
Nursing & Allied Health
Survey of what motivates nurses to choose traveler jobs: 1) better compensation; 2) adventure; 3) work-life balance; 4) ability to focus on patients, not politics.
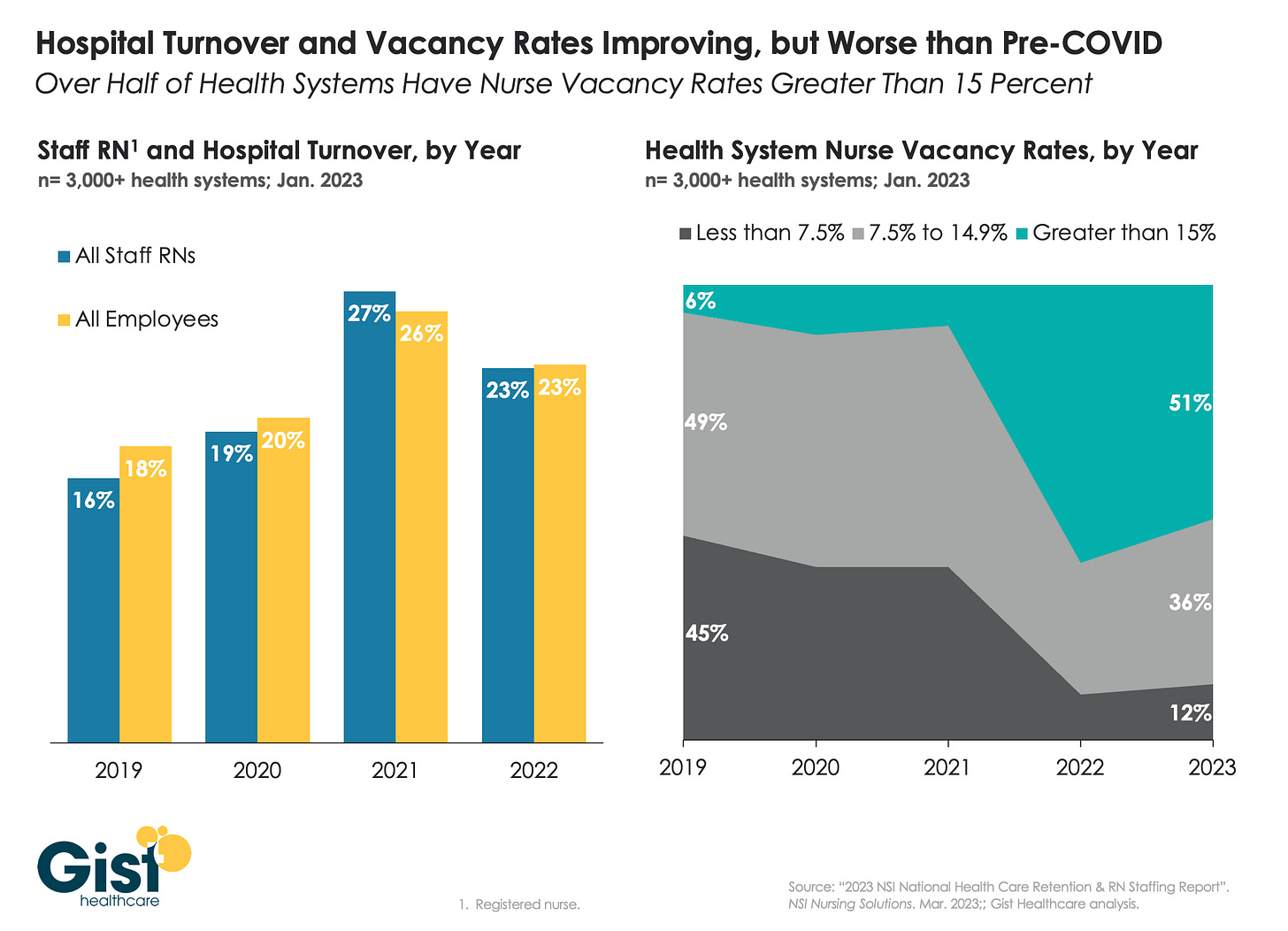
Per Gist Healthcare, the nursing turnover rate is decreasing, but still higher than pre-pandemic.
Countries around the world are competing with each other to attract nurses.